2026 Could Bring Higher Health Insurance Costs for Millions of Americans
 The costs of at least 350 drugs in the U.S. are expected to rise in 2026, according to a new analysis, despite many of the drugmakers pledging to offer more favorable prices under new Trump administration policies.
The costs of at least 350 drugs in the U.S. are expected to rise in 2026, according to a new analysis, despite many of the drugmakers pledging to offer more favorable prices under new Trump administration policies.
New data from the health care research firm 3 Axis Advisors, first reported by Reuters, found that a higher number of drugs would see price increases next year compared with last year, when more than 250 drugs were slated for markups.
President Donald Trump had floated a solution to ease the situation, but severe conservative backlash forced him to go back on his words. The Fox report states that there is a bipartisan plan in talks that seeks a three-year extension of the subsidies. It is similar to the Democrats’ plan, which is up for a vote in the House later this month. However, it would not be wise to pin one’s hopes on that vote… (Continue to full article)
US Drug Prices to Climb Again in 2026, Affecting 350 Branded Medicines
 US drug prices are set to rise again in 2026, with drugmakers planning increases on at least 350 branded medicines, according to new data from healthcare research firm 3 Axis Advisors.
US drug prices are set to rise again in 2026, with drugmakers planning increases on at least 350 branded medicines, according to new data from healthcare research firm 3 Axis Advisors.
The planned hikes will affect vaccines for COVID, RSV, and shingles, as well as major treatments like Pfizer’s cancer drug Ibrance, raising concerns for patients already paying some of the highest drug prices in the world.
The data shows the number of planned price increases is higher than last year.
At the same point in 2025, companies planned hikes on just over 250 drugs. For 2026, the median increase is about 4%, similar to this year, ET reported. These listed prices do not include rebates or discounts that drugmakers later negotiate with insurers or pharmacy benefit managers. The increases come even as President Trump continues to pressure pharmaceutical companies to lower US drug prices to levels closer to those in other wealthy countries.
Americans often pay nearly three times more for prescription medicines than patients in other developed nations… (Continue to full article)
Prescription Auto-Refills Are Switching Quantities Without Approval
 If you opened your mail-order pharmacy box this month only to find a 30-day supply of your maintenance meds instead of your usual 90-day bottle, you’ve hit a 2026 “Quantity Limit” wall. Across the country, prescription auto-refills are switching quantities without explicit patient approval, leaving many seniors to manage three times as many shipments. This isn’t a mistake by the pharmacist; it is a direct result of new 2026 insurance quantity limit policies designed to control costs as the new $2,000 Part D out-of-pocket cap goes into full effect. By shortening your supply, insurers can more closely monitor your “adherence” and reduce the financial risk of “wasted” medication that occurs when a patient’s dosage changes mid-quarter.
If you opened your mail-order pharmacy box this month only to find a 30-day supply of your maintenance meds instead of your usual 90-day bottle, you’ve hit a 2026 “Quantity Limit” wall. Across the country, prescription auto-refills are switching quantities without explicit patient approval, leaving many seniors to manage three times as many shipments. This isn’t a mistake by the pharmacist; it is a direct result of new 2026 insurance quantity limit policies designed to control costs as the new $2,000 Part D out-of-pocket cap goes into full effect. By shortening your supply, insurers can more closely monitor your “adherence” and reduce the financial risk of “wasted” medication that occurs when a patient’s dosage changes mid-quarter.
For those taking pain management or ADHD medications, the auto-refill switching quantities rules are even more stringent. New 2026 controlled substance regulations often cap initial fills at 30 days, even if a doctor writes for 90, to prevent “stockpiling” and diversion. If your state’s law or your pharmacy’s policy has updated its “Safety Edits” for the new year, the pharmacist is legally required to “auto-adjust” your quantity downward to comply with the most restrictive rule. This is part of a broader 2026 push to treat every controlled substance refill with the same scrutiny as a brand-new prescription.
The shift in auto-refills switching quantities is a frustrating “stealth change” that impacts your time, your budget, and your peace of mind. While insurers argue that 30-day fills reduce waste and improve safety, the reality for many seniors is a year filled with more trips to the pharmacy and more paperwork. By understanding the “75% rule” and proactively filing for “Quantity Limit Exceptions,” you can restore your 90-day supply and reduce the stress of your monthly medication management. Don’t let an “auto-adjust” algorithm dictate how you manage your health and your time in the new year… (Continue to full article)

Kiss mah…
AARP Sounds the Alarm on Social Security and Medicare in 2026
As 2026 approaches, millions of Americans preparing for retirement are facing crucial updates to two of the nation’s most important safety-net programs: Social Security and Medicare. Advocacy group AARP, representing over 120 million Americans age 50 and older, has delivered a clear message: benefits are changing, costs are rising, and retirees need to understand what it all means for their financial future.
While Social Security benefits are increasing, Medicare premiums are rising even faster, and for many retirees, that means less net income despite the COLA
The standard monthly premium for Medicare Part B — which covers doctor visits and outpatient care — will jump from $185 in 2025 to $202.90 in 2026, an increase of nearly 10%. The annual deductible for Part B also rises to $283.
These increases can significantly erode the effective value of the Social Security COLA, especially since many beneficiaries have their Medicare premiums deducted directly from their benefit checks… (Continue to full article)
UnitedHealth Boots 1 Million Seniors in a Medicare Shakeup Not Seen in 20 Years
 UnitedHealth’s decision to push roughly one million seniors out of its Medicare Advantage products marks a break from the incremental tweaks that usually define this market. For older Americans who built their budgets and care relationships around these plans, the shift is not an abstract business story but a direct hit to how they will access doctors, drugs, and hospitals next year. I see it as the clearest sign in two decades that the balance of power between giant insurers and aging consumers is tilting again, and not in favor of retirees.
UnitedHealth’s decision to push roughly one million seniors out of its Medicare Advantage products marks a break from the incremental tweaks that usually define this market. For older Americans who built their budgets and care relationships around these plans, the shift is not an abstract business story but a direct hit to how they will access doctors, drugs, and hospitals next year. I see it as the clearest sign in two decades that the balance of power between giant insurers and aging consumers is tilting again, and not in favor of retirees.
When a company the size of UnitedHealth moves, the ripple effects rarely stay contained, and the projected loss of roughly one million Medicare Advantage members is closer to a tidal surge than a wave. Executives have signaled that Medicare Advantage enrollment will shrink by about 1 million people, a figure that reflects both members being pushed out of nonrenewed plans and others walking away from slimmer benefits.
In practical terms, that means hundreds of thousands of households will be forced to re-shop coverage, re-check drug formularies, and re-learn which doctors are in network, all at an age when administrative friction can be as punishing as a medical bill… (Continue to full article)
 The modern American health insurance system didn’t emerge because someone designed it thoughtfully, and it shows. It evolved from a series of political, economic, and cultural accidents beginning largely around the period of World War II. As with many political redistribution schemes, once underway, the system has snowballed into the unsustainable trajectory we see today.
The modern American health insurance system didn’t emerge because someone designed it thoughtfully, and it shows. It evolved from a series of political, economic, and cultural accidents beginning largely around the period of World War II. As with many political redistribution schemes, once underway, the system has snowballed into the unsustainable trajectory we see today.
 On December 5, 2025, the CDC’s ACIP committee voted 8-3 to end the automatic Hep B shot for every newborn. For the first time since 1991 hospitals can no longer treat every baby as if they were born to an infected mother.
On December 5, 2025, the CDC’s ACIP committee voted 8-3 to end the automatic Hep B shot for every newborn. For the first time since 1991 hospitals can no longer treat every baby as if they were born to an infected mother. Liz Moore’s son Bodin struggled from birth: feeding and sleeping problems, followed by developmental and academic delays, social awkwardness, and finally an ADHD diagnosis at age 6.
Liz Moore’s son Bodin struggled from birth: feeding and sleeping problems, followed by developmental and academic delays, social awkwardness, and finally an ADHD diagnosis at age 6.  The costs of at least 350 drugs in the U.S. are expected to rise in 2026, according to a new analysis, despite many of the drugmakers pledging to offer more favorable prices under new Trump administration policies.
The costs of at least 350 drugs in the U.S. are expected to rise in 2026, according to a new analysis, despite many of the drugmakers pledging to offer more favorable prices under new Trump administration policies. US drug prices are set to rise again in 2026, with drugmakers planning increases on at least 350 branded medicines, according to new data from healthcare research firm 3 Axis Advisors.
US drug prices are set to rise again in 2026, with drugmakers planning increases on at least 350 branded medicines, according to new data from healthcare research firm 3 Axis Advisors. If you opened your mail-order pharmacy box this month only to find a 30-day supply of your maintenance meds instead of your usual 90-day bottle, you’ve hit a 2026 “Quantity Limit” wall. Across the country, prescription auto-refills are switching quantities without explicit patient approval, leaving many seniors to manage three times as many shipments. This isn’t a mistake by the pharmacist; it is a direct result of new 2026 insurance quantity limit policies designed to control costs as the new $2,000 Part D out-of-pocket cap goes into full effect. By shortening your supply, insurers can more closely monitor your “adherence” and reduce the financial risk of “wasted” medication that occurs when a patient’s dosage changes mid-quarter.
If you opened your mail-order pharmacy box this month only to find a 30-day supply of your maintenance meds instead of your usual 90-day bottle, you’ve hit a 2026 “Quantity Limit” wall. Across the country, prescription auto-refills are switching quantities without explicit patient approval, leaving many seniors to manage three times as many shipments. This isn’t a mistake by the pharmacist; it is a direct result of new 2026 insurance quantity limit policies designed to control costs as the new $2,000 Part D out-of-pocket cap goes into full effect. By shortening your supply, insurers can more closely monitor your “adherence” and reduce the financial risk of “wasted” medication that occurs when a patient’s dosage changes mid-quarter.
 UnitedHealth’s decision to push roughly one million seniors out of its Medicare Advantage products marks a break from the incremental tweaks that usually define this market. For older Americans who built their budgets and care relationships around these plans, the shift is not an abstract business story but a direct hit to how they will access doctors, drugs, and hospitals next year. I see it as the clearest sign in two decades that the balance of power between giant insurers and aging consumers is tilting again, and not in favor of retirees.
UnitedHealth’s decision to push roughly one million seniors out of its Medicare Advantage products marks a break from the incremental tweaks that usually define this market. For older Americans who built their budgets and care relationships around these plans, the shift is not an abstract business story but a direct hit to how they will access doctors, drugs, and hospitals next year. I see it as the clearest sign in two decades that the balance of power between giant insurers and aging consumers is tilting again, and not in favor of retirees. The root cause of our current health care affordability crisis is a broken market structure on the supply side resulting in out-of-control costs. The (apparently) core public policy issues: insurance, pre-existing conditions, employment linkage, lack of portability, the extent of coverage, denials, out of pocket costs, and deductibles would all become non-issues if health care was a normal expense that people could afford out of their income.
The root cause of our current health care affordability crisis is a broken market structure on the supply side resulting in out-of-control costs. The (apparently) core public policy issues: insurance, pre-existing conditions, employment linkage, lack of portability, the extent of coverage, denials, out of pocket costs, and deductibles would all become non-issues if health care was a normal expense that people could afford out of their income. 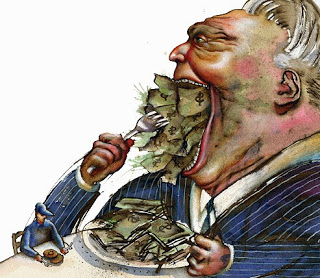
 A new flu variant known as subclade K is on the rise across the country. Although a spike in this particular strain of influenza, referred to by some as a “super flu,” has been recorded, symptoms remain similar to the most common form of flu called influenza A. Doctors say vaccination is the best way to avoid hospitalization or complications for those at risk.
A new flu variant known as subclade K is on the rise across the country. Although a spike in this particular strain of influenza, referred to by some as a “super flu,” has been recorded, symptoms remain similar to the most common form of flu called influenza A. Doctors say vaccination is the best way to avoid hospitalization or complications for those at risk.  The cookware we use, the plates we eat from, and the food we put in our bodies every day may seem mundane, but they can be significant sources of chronic toxins.
The cookware we use, the plates we eat from, and the food we put in our bodies every day may seem mundane, but they can be significant sources of chronic toxins. Managing ulcerative colitis typically means navigating the unpredictable – disease flares, personal trigger foods, and the challenges of dietary restrictions. However, emerging evidence suggests a simple intervention – drinking eight ounces of coconut water twice daily – may help some patients achieve remission.
Managing ulcerative colitis typically means navigating the unpredictable – disease flares, personal trigger foods, and the challenges of dietary restrictions. However, emerging evidence suggests a simple intervention – drinking eight ounces of coconut water twice daily – may help some patients achieve remission. 
 Many forms of cancer are devastating. But pancreatic cancer is one of the most deadly and aggressive forms there is. There are several reasons for this, including its stealthy progression, rapid metastasis (the way it spreads), and late detection. In fact, early detection is so rare there’s a five-year survival rate of 13.3%.
Many forms of cancer are devastating. But pancreatic cancer is one of the most deadly and aggressive forms there is. There are several reasons for this, including its stealthy progression, rapid metastasis (the way it spreads), and late detection. In fact, early detection is so rare there’s a five-year survival rate of 13.3%.
 Popcorn is more than just a movie’s best friend; in fact, it’s actually quite good for you. We’re not just talking that “skinny pop” stuff that cuts both the calories and flavors in half. Your average bowl of popcorn is surprisingly healthy.
Popcorn is more than just a movie’s best friend; in fact, it’s actually quite good for you. We’re not just talking that “skinny pop” stuff that cuts both the calories and flavors in half. Your average bowl of popcorn is surprisingly healthy. Everyday plastic exposures can affect hormones and long-term health, but simple steps can help reduce your risk.
Everyday plastic exposures can affect hormones and long-term health, but simple steps can help reduce your risk. A deadly quad-demic is taking shape in the US as the months get colder and people gather indoors, threatening to overwhelm hospitals, disrupt children’s education and pose a deadly risk to vulnerable seniors.
A deadly quad-demic is taking shape in the US as the months get colder and people gather indoors, threatening to overwhelm hospitals, disrupt children’s education and pose a deadly risk to vulnerable seniors.