Gender at your fingertips
The sources for the statistics we use are selected for their reliability. We mostly use peer-reviewed papers; however, we occasionally refer to government-commissioned studies, authoritative bodies' submissions to governmental commissions, published books, or doctoral theses. In a few cases, we provide references for the purpose of debunking unreliable data.
As this is an emerging field of research, the information on this page may develop over time. Statistics for the transgender population are often difficult to quantify as different definitions are used to describe the term "transgender". Our focus is to underpin the statements we provide with sound research. We know that these statements cannot comprehensively cover every topic; however, this initiative is intended to bring some much-needed clarity to this area of study.
Stats For Gender is powered by Genspect, an organization that advocates for a non-medicalised approach to gender dysphoria.
Filter by topic
…or by keyword
Showing 154 posts
-
NHS gender clinics do not meet quality assurance standards.
An operational and delivery review1 of adult gender clinics in England found that clinics lacked patient outcome data, had limited data reporting of inconsistent quality, and had minimal clinical audit. These failings put the clinics outside standard NHS quality assurance expectations.
These clinics also showed no signs of responding to the changing demographics of their referrals. Clinics made little effort to respond to the needs of this changing cohort, which was younger and more female than had previously been the case.
Some clinics reportedly carried out little or no knowledge-sharing or quality improvement work. Senior clinical leadership also steered some clinicians away from appropriate clinical curiosity, limiting opportunities to improve patient outcomes. In addition, many clinics were not well overseen by their local trust boards, nor by NHS England.
- Levy D, Operational and delivery review of NHS adult gender dysphoria clinics in England. https://www.england.nhs.uk/publication/operational-and-delivery-review-of-nhs-adult-gender-dysphoria-clinics-in-england/ ↩︎
-
All-cause mortality is higher for women taking testosterone than for women in general.
A retrospective cohort study1 of patients at an Amsterdam gender clinic found that all-cause mortality increased for females receiving testosterone and continued to increase over time. Women taking testosterone had an overall Standard Mortality Ratio (SMR) of 1.8 compared to women in general. Deaths from non-natural causes were especially high.
- de Blok CJ, Wiepjes CM, van Velzen DM, Staphorsius AS, Nota NM, Gooren LJ, Kreukels BP, den Heijer M. Mortality trends over five decades in adult transgender people receiving hormone treatment: a report from the Amsterdam cohort of gender dysphoria. Lancet Diabetes and Endocrinology. 2021 Oct;9(10):663-670. doi: 10.1016/S2213-8587(21)00185-6. Epub 2021 Sep 2. PMID: 34481559. ↩︎
-
All-cause mortality is higher for males taking estrogen than for men in general.
A retrospective cohort study1 of patients at an Amsterdam gender clinic found that all-cause mortality increased within a few years of beginning estrogen treatment and continued to increase over time. Men taking estrogen had an overall Standard Mortality Ratio (SMR) of 1.8 compared to men in general. The major causes of death included cardiovascular disease (21%), cancer (32%), infection-related disease (5%), and suicide (7.5%).
- de Blok CJ, Wiepjes CM, van Velzen DM, Staphorsius AS, Nota NM, Gooren LJ, Kreukels BP, den Heijer M. Mortality trends over five decades in adult transgender people receiving hormone treatment: a report from the Amsterdam cohort of gender dysphoria. Lancet Diabetes and Endocrinology. 2021 Oct;9(10):663-670. doi: 10.1016/S2213-8587(21)00185-6. Epub 2021 Sep 2. PMID: 34481559. ↩︎
-
Around one in six young people treated with cross sex hormones ceased treatment.
An exploratory study1 of adolescents and young adults in Canada and the US found that 16.8% of those receiving “gender affirming medical treatment” (puberty blockers and cross sex hormones) stopped “treatment” within around five years of declaring a “trans” or “non binary” identity.
Of those who discontinued treatment, 37.3% did so for health reasons. 32% ended treatment due to a change in gender identity. 12% were persuaded by health professionals or a partner to explore different ways of approaching their gender dysphoria.
Stopping treatment was associated with having a “non binary” identity. Both continuing and non-continuing cohorts had a mean age of 16.1 when “coming out”, but those discontinuing treatment were slightly older (22.1 vs. 20.9.)
- MacKinnon KR, Jeyabalan T, Strang JF, Delgado-Ron JA, Lam JSH, Gould WA, Cooper A, Salway T. Discontinuation of Gender-Affirming Medical Treatments: Prevalence and Associated Features in a Nonprobabilistic Sample of Transgender and Gender-Diverse Adolescents and Young Adults in Canada and the United States. Journal of Adolescent Health. 2024 Oct;75(4):569-577. doi: 10.1016/j.jadohealth.2024.05.015. Epub 2024 Jun 28. PMID: 38944803. ↩︎
-
Bone mineral density that declines during puberty blockade may not fully recover with cross-sex hormone treatment.
A cohort study1 of trans-identified people who had received puberty blockers and long-term cross sex hormones found that bone mineral density z-scores (which compare the patient with age- and sex-typical values) fell during puberty blockade, and did not fully recover following over a decade of cross-sex hormone treatment. This was especially the case for the lumbar spine of males receiving estrogen.
It is also notable that, of the original 143 eligible participants, only 75 completed this research. Of those who left the cohort, 6 (4%) had discontinued cross-sex hormone treatment and 27 (19%) could not be reached. These figures are consistent with high loss to follow up in other studies of so-called “gender-affirming care.”

- van der Loos MATC, Vlot MC, Klink DT, Hannema SE, den Heijer M, Wiepjes CM. Bone Mineral Density in Transgender Adolescents Treated With Puberty Suppression and Subsequent Gender-Affirming Hormones. JAMA Pediatrics. 2023 Dec 1;177(12):1332-1341. doi: 10.1001/jamapediatrics.2023.4588. PMID: 37902760; PMCID: PMC10616766. ↩︎
-
Trans-identified people have higher than average rates of all mental illnesses.
A study1 of the medical records of 10,270 trans-identified patients found that 58% had at least one psychiatric diagnosis. This compares to just 13.6% of patients without trans identities. Trans-identified patients showed greater prevalence of every psychiatric condition queried, with major depressive disorder and generalized anxiety disorder being the most common diagnoses (31% and 12%, respectively). There was also an increased lifetime prevalence of bipolar disorder (11%) and psychotic disorders (4.7% overall, 2.5% for schizophrenia and 2.2% for schizoaffective disorder) in trans-identified patients.

- Wanta JW, Niforatos JD, Durbak E, Viguera A, Altinay M. Mental Health Diagnoses Among Transgender Patients in the Clinical Setting: An All-Payer Electronic Health Record Study. Transgender Health. 2019 Nov 1;4(1):313-315. doi: 10.1089/trgh.2019.0029. PMID: 31701012; PMCID: PMC6830528. ↩︎
-
Boys receiving puberty blockers for gender dysphoria experienced irreversible changes to their testes.
A histological analysis1 of testicular tissue taken from boys receiving puberty blockers for gender dysphoria showed that the tissue showed abnormal development that was likely to be irreversible.

Samples were gathered as part of “fertility preservation surgery,” in which testicular tissue is harvested and preserved in hope that it will be able to produce sperm later. Every boy with gender dysphoria in the study had elected for this surgery due to inability or reluctance to ejaculate. This suggests the possible presence of various psychological and physical conditions that are unexplored in the research.
- Murugesh V, Ritting M, Salem S, Aalam SMM, Garcia J, Chattha AJ, Zhao Y, Knapp DJ, Kalthur G, Granberg CF, Kannan N. Puberty Blocker and Aging Impact on Testicular Cell States and Function. bioRxiv [Preprint]. 2024 Mar 27:2024.03.23.586441. Doi: 10.1101/2024.03.23.586441. PMID: 38585884; PMCID: PMC10996503. ↩︎
-
Critical media coverage of “gender-affirming care” was associated with a decline in gender clinic referrals.
An analysis1 of gender clinic referrals in Sweden found an association between “negative” media coverage of “gender-affirming care” – specifically the “Trans Train”2 documentary – and a decrease of 25.4% in referrals to pediatric gender clinics.
- Indremo M, Jodensvi AC, Arinell H, Isaksson J, Papadopoulos FC. Association of Media Coverage on Transgender Health With Referrals to Child and Adolescent Gender Identity Clinics in Sweden. JAMA Netw Open. 2022;5(2):e2146531. doi:10.1001/jamanetworkopen.2021.46531 ↩︎
- https://youtu.be/MVEZ7gELcgY?si=6uc6DZBmGsKlXXQ8 ↩︎
-
Psychological effects of puberty blockers on young people may be worse than placebo.
An analysis1 comparing psychological effects of puberty blockers on teenagers with gender dysphoria with existing research on placebo effects for various mental health conditions found that placebo effects appeared to be at least as strong as the effect of puberty blockers, if not stronger.
- https://sex-matters.org/wp-content/uploads/2022/12/Teenagers-medication-vs-placebo.pdf ↩︎
-
Depression symptoms got worse in children taking puberty blockers.
In a study1 of 94 children with gender dysphoria, aged 8-16 and beginning to take puberty blockers, depression symptoms were more likely to get worse than to improve over two years of treatment. Scores on the Beck Depression Inventory (BDI-Y) went from 72% average, 10% mildly elevated, 10% moderately elevated, and 8% severely elevated at baseline to 75% average, 7% mildly elevated, 14% moderately elevated, and 9% severely elevated after 24 months.
This study was conducted from 2016 to 2021 by Dr. Johanna Olson-Kennedy. In 2024, the New York Times reported2 Dr. Olson-Kennedy saying that publication of this research had been delayed because she feared that research showing that puberty blockers did not improve patients’ mental health would be “weaponized” against the use of puberty blockers by opponents of the practice. The report appeared as a pre-print, not peer-reviewed, in May 2025.
- Johanna Olson-Kennedy, Liyuan Wang, Carolyn F. Wong, Diane Chen, Diane Ehrensaft, Marco A. Hidalgo, Amy C. Tishelman, Yee-Ming Chan, Robert Garofalo, Asa E. Radix, Stephen M. Rosenthal, Emotional Health of Transgender Youth 24 Months After Initiating Gender-Affirming Hormone Therapy, Journal of Adolescent Health, Volume 77, Issue 1, 2025, Pages 41-50, ISSN 1054-139X, https://doi.org/10.1016/j.jadohealth.2024.11.014. ↩︎
- https://www.nytimes.com/2024/10/23/science/puberty-blockers-olson-kennedy.html
↩︎
-
Women taking GnRH agonists for endometriosis experienced memory problems during treatment.
A study1 of women taking GnRH agonists (a/k/a “puberty blockers”) to treat endometriosis found that 31% had “mild” memory problems, 25% had “moderate” problems, and 19% had “marked” problems. Problems were mainly with prospective and short-term memory.
- Christopher Newton, Dianne Slota, Albert A. Yuzpe, Ian S. Tummon, Memory complaints associated with the use of gonadotropin-releasing hormone agonists: a preliminary study, Fertility and Sterility, Volume 65, Issue 6, 1996. ISSN 0015-0282. https://doi.org/10.1016/S0015-0282(16)58351-4. ↩︎
-
The IQ of girls given puberty blockers for precocious puberty fell by eight points.
A study1 of 15 girls treated with puberty blockers for central precocious puberty showed that IQ fell by around eight points. The average fell from 102 (55th percentile) to 94 (34th percentile). Two patients were held back a year at school.
In another study2 of 30 children experiencing early puberty and treated with puberty blockers, IQ fell by around seven points.
- Wojniusz S, Callens N, Sütterlin S, Andersson S, De Schepper J, Gies I, Vanbesien J, De Waele K, Van Aken S, Craen M, Vögele C, Cools M, Haraldsen IR. Cognitive, Emotional, and Psychosocial Functioning of Girls Treated with Pharmacological Puberty Blockage for Idiopathic Central Precocious Puberty. Frontiers in Psychology. 2016 Jul 12;7:1053. doi: 10.3389/fpsyg.2016.01053. PMID: 27462292; PMCID: PMC4940404. ↩︎
- Mul D, Versluis-den Bieman HJ, Slijper FM, Oostdijk W, Waelkens JJ, Drop SL. Psychological assessments before and after treatment of early puberty in adopted children. Acta Paediatrica. 2001 Sep;90(9):965-71. doi: 10.1080/080352501316978011. PMID: 11683207. ↩︎
-
IQ fell in a male patient whose puberty was blocked due to gender distress.
A case study1 of a male patient whose puberty was blocked at age 11 showed a decline in several measurements of intelligence over the following three years, including decline of 10 points in global IQ and 15 points in verbal comprehension.
Verbal comprehension showed a continuous decline. Other measurements showed some improvement after an initial decline, but never recovered to baseline levels. Processing speed index scores initially improved, but then fell below baseline.

- Schneider MA, Spritzer PM, Soll BMB, Fontanari AMV, Carneiro M, Tovar-Moll F, Costa AB, da Silva DC, Schwarz K, Anes M, Tramontina S, Lobato MIR. Brain Maturation, Cognition and Voice Pattern in a Gender Dysphoria Case under Pubertal Suppression. Frontiers in Human Neuroscience. 2017 Nov 14;11:528. doi: 10.3389/fnhum.2017.00528. PMID: 29184488; PMCID: PMC5694455. ↩︎
-
Animal studies suggest puberty blockers may impair brain development, sometimes irrevocably.
A review1 of studies of the effect of puberty blockers on animals (sheep, mice, macaque monkeys) suggests that brain development and neurological functioning may be compromised by the treatment. In some cases, hormone replacement (i.e. testosterone replacement in male sheep given GnRH agonists) did not mitigate or undo the observed changes. A variety of sex-specific effects were also observed.
- Baxendale S. The impact of suppressing puberty on neuropsychological function: a review. Acta Paediatrica. 2024; 113(6): 1156-1167. doi:10.1111/apa.17150 ↩︎
-
More patients on puberty blockers saw their distress deteriorate than improve.
A study1 of children from 12-15 receiving puberty blockers via the Gender Identity and Development Service showed that 37-70% of patients showed no improvement in levels of distress. 15-34% showed deterioration, while only 9-29% showed improvement.
The highest rate of deterioration (34%) was recorded at the 12 month evaluation, when the sample size was at its largest. Evaluations at 24 and 36 months were affected by significant loss to follow-up, which compromises the data.
- McPherson, S., & Freedman, D. E. P. (2023). Psychological Outcomes of 12–15-Year-Olds with Gender Dysphoria Receiving Pubertal Suppression in the UK: Assessing Reliable and Clinically Significant Change. Journal of Sex & Marital Therapy, 50(3), 315–325. https://doi.org/10.1080/0092623X.2023.2281986 ↩︎
-
94% of females taking testosterone experience pelvic floor dysfunction.
In a study1 of 68 women taking testosterone, 94.1% had some form of pelvic floor dysfunction. 86.7% had urinary symptoms. Other problems included storage symptoms (69.1%), sexual dysfunction (52.9%), anorectal symptoms (45.6%), and flatal incontinence (39.7%.)
- da Silva LMB, Freire SND, Moretti E, Barbosa L. Pelvic Floor Dysfunction in Transgender Men on Gender-affirming Hormone Therapy: A Descriptive Cross-sectional Study. International Urogynecology Journal. 2024 May;35(5):1077-1084. doi: 10.1007/s00192-024-05779-3. Epub 2024 Apr 25. PMID: 38662108. ↩︎
-
Rates of suicidality and self-harm did not improve in teenagers taking puberty blockers.
In a prospective study1 of patients aged 12-15 referred to University College Hospital, London by the Gender Identity Development Service, patients on puberty blockers showed no change in rates of suicidality or self-harm.
This study is compromised by the lack of follow-up once patients reached the age of 16, meaning there were significant effective drop-out rates at 24 and 36 months.
- Carmichael P, Butler G, Masic U, Cole TJ, De Stavola BL, Davidson S, Skageberg EM, Khadr S, Viner RM. Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS One. 2021 Feb 2;16(2):e0243894. doi: 10.1371/journal.pone.0243894. PMID: 33529227; PMCID: PMC7853497. ↩︎
-
The height of teenagers taking puberty blockers did not increase at an age-appropriate rate.
In a prospective study1 of patients aged 12-15 referred to University College Hospital, London by the Gender Identity Development Service, patients on puberty blockers did grow taller, but not by as much as others in their age group.
- Carmichael P, Butler G, Masic U, Cole TJ, De Stavola BL, Davidson S, Skageberg EM, Khadr S, Viner RM. Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS One. 2021 Feb 2;16(2):e0243894. doi: 10.1371/journal.pone.0243894. PMID: 33529227; PMCID: PMC7853497. ↩︎
-
Teenagers taking puberty blockers report more negative mood changes over time.
In a prospective study1 of patients aged 12-15 referred to University College Hospital, London by the Gender Identity Development Service, patients reported increases in negative mood and decreases in positive mood over time since beginning puberty blockage.
This study is compromised by the lack of follow-up once patients reached the age of 16, meaning there were significant effective drop-out rates at 24 and 36 months.

- Carmichael P, Butler G, Masic U, Cole TJ, De Stavola BL, Davidson S, Skageberg EM, Khadr S, Viner RM. Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS One. 2021 Feb 2;16(2):e0243894. doi: 10.1371/journal.pone.0243894. PMID: 33529227; PMCID: PMC7853497. ↩︎
-
The bone mineral density of teenagers taking puberty blockers did not increase to age-appropriate levels
In a prospective study1 of patients aged 12-15 referred to University College Hospital, London by the Gender Identity Development Service, bone mineral density (BMD) in the hip showed no change from baseline over 36 months. Spinal BMD showed some increase at 24 months, but at no point did BMD show an age-appropriate increase.
This study is compromised by the lack of follow-up once patients reached the age of 16, meaning there were significant effective drop-out rates at 24 and 36 months.
- Carmichael P, Butler G, Masic U, Cole TJ, De Stavola BL, Davidson S, Skageberg EM, Khadr S, Viner RM. Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS One. 2021 Feb 2;16(2):e0243894. doi: 10.1371/journal.pone.0243894. PMID: 33529227; PMCID: PMC7853497. ↩︎
-
Puberty blockers did not improve psychological functioning of GIDS patients.
In a prospective study1 of patients aged 12-15 referred to University College Hospital, London by the Gender Identity Development Service, psychological functioning (measured using the Child Behaviour Checklist) was not shown to improve 12, 24 or 36 months after beginning puberty blockage.
This study is compromised by the lack of follow-up once patients reached the age of 16, meaning there were significant effective drop-out rates at 24 and 36 months.
- Carmichael P, Butler G, Masic U, Cole TJ, De Stavola BL, Davidson S, Skageberg EM, Khadr S, Viner RM. Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS One. 2021 Feb 2;16(2):e0243894. doi: 10.1371/journal.pone.0243894. PMID: 33529227; PMCID: PMC7853497. ↩︎
-
Men taking exogenous estrogen may be at higher risk of branch retinal vein occlusion.
In a case study1 of a man taking “gender-affirming” estrogen, a plausible causal link was suggested between exogenous estrogen and branch retinal vein occlusion (BRVO), based chiefly on existing established links between estrogen and cardiovascular risk. The study also suggests that trans-identified patients may be unwilling to stop using estrogen even when experiencing BRVO.
- Andzembe V, Miere A, Zambrowski O, Glacet-Bernard A, Souied EH. Branch retinal vein occlusion secondary to hormone replacement therapy in a transgender woman. J Fr Ophtalmol. 2023 Feb;46(2):148-151. doi: 10.1016/j.jfo.2022.07.024. Epub 2023 Jan 4. PMID: 36609071. ↩︎
-
There may be a causal link between exogenous testosterone and idiopathic intracranial hypertension (IIH.)
In a study1 of a series of cases of females taking “gender-affirming” testosterone, a plausible causal relationship was suggested between the exogenous testosterone and the precipitation of symptoms of idiopathic intracranial hypertension (IIH). Onset of IIH was between ten weeks and ten years after beginning testosterone treatment.
- Gutkind NE, Tse DT, Johnson TE, Tse BC. Idiopathic Intracranial Hypertension in Female-to-Male Transgender Patients on Exogenous Testosterone Therapy. Ophthalmic Plastic and Reconstructive Surgery. 2023 Sep-Oct 01;39(5):449-453. doi: 10.1097/IOP.0000000000002344. Epub 2023 Feb 21. PMID: 36804335; PMCID: PMC10440365. ↩︎
-
Females taking testosterone may be at increased risk of intracranial hypertension.
A case study1 of idiopathic intracranial hypertension (IIH) in a woman taking “gender-affirming” testosterone suggests that there may be a causal link between elevated testosterone and the onset and progression of IIH.
- Hornby C, Mollan SP, Mitchell J, Markey KA, Yangou A, Wright BLC, O’Reilly MW, Sinclair AJ. What Do Transgender Patients Teach Us About Idiopathic Intracranial Hypertension? Neuroophthalmology. 2017 May 10;41(6):326-329. doi: 10.1080/01658107.2017.1316744. PMID: 29238388; PMCID: PMC5706971. ↩︎
-
Males taking estrogen may be at risk of keratoconus.
A case study1 of a 28 year old man taking “gender-affirming” estrogen suggested that such treatment may accelerate the progression of keratoconus.
- Carli M. Deitel, Kevin H. Chen, Ian C. Uber, Possible association of keratoconus progression with gender-affirming hormone therapy: A case report, American Journal of Ophthalmology Case Reports, Volume 30, 2023, 101850, ISSN 2451-9936, https://doi.org/10.1016/j.ajoc.2023.101850. ↩︎
-
People taking cross-sex hormones may be at risk of certain ocular problems.
A small study1 of patients at one ophthalmology clinic found that female patients taking testosterone seemed to be at risk of idiopathic intracranial hypertension (IIH), while male patients taking estrogen were more likely to experience chorioretinal conditions (chorioretinitis and central serious chorioretinopathy.) Causality could not be demonstrated and prevalence could not be estimated.
- Nieves-Ríos C, Pulido JS, Thornton S, Dunn JP, Procopio RA, Oliver AL, Lee D, Edwards R, Sergott RC, Moster ML. Instances of ocular findings in transgender patients undergoing hormonal therapy. American Journal of Ophthalmology Case Reports. 2023 Nov 28;32:101965. doi: 10.1016/j.ajoc.2023.101965. PMID: 38077787; PMCID: PMC10701352. ↩︎
-
Rates of autism are much higher in trans-identified people.
In an analysis1 of five large datasets, “trangender and gender diverse” individuals were 3.03 to 6.36 times more likely to be autistic than those who do not claim an alternative gender identity.
- Warrier, V., Greenberg, D.M., Weir, E. et al. Elevated rates of autism, other neurodevelopmental and psychiatric diagnoses, and autistic traits in transgender and gender-diverse individuals. Nature Communications 11, 3959 (2020). https://doi.org/10.1038/s41467-020-17794-1 ↩︎
-
43% of trans-identified people experience anxiety. The figure is higher for females.
A systematic review1 of 71 studies, comprising 73,565 transgender individuals from 23 countries, found a global pooled prevalence of anxiety of 43%. Prevalence was 59% amongst “non-binary” people and 44% for “transmasculine” people.
- Oliveira Teles, D., Alves de Oliveira, R., de Mendonça Figueirêdo Coelho, M., Bezerra Pinheiro, A. K., & Lannes Fernandes, F. (2025). Worldwide prevalence of anxiety in transgender persons: Systematic review with meta-analysis. International Journal of Transgender Health, 1–23. https://doi.org/10.1080/26895269.2025.2498753 ↩︎
-
More than 80% of trans-identified young people experienced depressive mood, and more than half had considered suicide.
In a national quantitative cross-sectional survey1 of more than 25,000 “LGBQ” people, aged between 13 and 24 years, in the U.S., 82% reported experiencing depressive mood. 54% said they had seriously considered suicide, and 28% reported attempting suicide, in the last 12 months. Across all groups, females were more likely to experience depression, suicidality and attempted suicide than males. Participants with “trans” and “non-binary” identities were about twice as likely to report depressive mood and having considered suicide, and about one and a half times as likely to report a suicide attempt.
- Price-Feeney, Myeshia et al., Understanding the Mental Health of Transgender and Nonbinary Youth, Journal of Adolescent Health, Volume 66, Issue 6, 684 – 690 ↩︎
-
“Gender questioning” adolescents may have very high rates of disordered eating.
In a cross-sectional study1 of 660 Australian adolescents described as “trans,” “non-binary” and “gender questioning,” adolescents who reported feeling unsure about their “gender identity” had the highest rates of nearly all symptoms of anorexia and bulimia.
- Kerr JA, Paine J, Thrower E, Hoq M, Mollica C, Sawyer SM, Azzopardi PS, Pang KC. Prevalence of Eating Disorder Symptoms in Transgender and Gender Diverse Adolescents Presenting for Gender-Affirming Care. Journal of Adolescent Health. 2024 Apr;74(4):850-853. doi: 10.1016/j.jadohealth.2023.11.396. Epub 2024 Jan 9. PMID: 38206224.
↩︎
- Kerr JA, Paine J, Thrower E, Hoq M, Mollica C, Sawyer SM, Azzopardi PS, Pang KC. Prevalence of Eating Disorder Symptoms in Transgender and Gender Diverse Adolescents Presenting for Gender-Affirming Care. Journal of Adolescent Health. 2024 Apr;74(4):850-853. doi: 10.1016/j.jadohealth.2023.11.396. Epub 2024 Jan 9. PMID: 38206224.
-
Nearly a quarter of adolescents seeking “gender-affirming care” report symptoms of anorexia.
In a cross-sectional study1 of 660 Australian adolescents described as “trans,” “non-binary” and “gender questioning,” 23.9% reported symptoms of anorexia. Prevalence of disordered eating was more common in female patients than in male, regardless of whether they identified as trans or non-binary.
- Kerr JA, Paine J, Thrower E, Hoq M, Mollica C, Sawyer SM, Azzopardi PS, Pang KC. Prevalence of Eating Disorder Symptoms in Transgender and Gender Diverse Adolescents Presenting for Gender-Affirming Care. Journal of Adolescent Health. 2024 Apr;74(4):850-853. doi: 10.1016/j.jadohealth.2023.11.396. Epub 2024 Jan 9. PMID: 38206224. ↩︎
-
Young people with “trans” identities are much more likely to have an eating disorder.
A study1 of data concerning 289,024 students from 223 U.S. universities found that students with a “trans” identity were almost four times more likely to have a self-reported eating disorder (OR: 4.62, 95% CI: 3.41-6.26) than their straight female peers. They were also about twice as likely to report past month use of diet pills (OR: 2.05, 95% CI: 1.48-2.83) and vomiting or laxatives (OR: 2.46, 95% CI: 1.83-3.30).
- Diemer EW, Grant JD, Munn-Chernoff MA, Patterson DA, Duncan AE. Gender Identity, Sexual Orientation, and Eating-Related Pathology in a National Sample of College Students. Journal of Adolescent Health. 2015 Aug;57(2):144-9. doi: 10.1016/j.jadohealth.2015.03.003. Epub 2015 Apr 28. PMID: 25937471; PMCID: PMC4545276. ↩︎
-
Up to half of trans-identified children show disordered eating.
In an analysis1 of research conducted in 2022-23, 20-50% of children expressing a “trans” identity reported engaging in some form of disordered eating. More than 30% screened positive for eating disorder symptoms, and up to 12% had received an eating disorder diagnosis.
- Keski-Rahkonen A. Eating disorders in transgender and gender diverse people: characteristics, assessment, and management. Current Opinion in Psychiatry. 2023 Nov 1;36(6):412-418. doi: 10.1097/YCO.0000000000000902. Epub 2023 Aug 29. PMID: 37781981.
↩︎
- Keski-Rahkonen A. Eating disorders in transgender and gender diverse people: characteristics, assessment, and management. Current Opinion in Psychiatry. 2023 Nov 1;36(6):412-418. doi: 10.1097/YCO.0000000000000902. Epub 2023 Aug 29. PMID: 37781981.
-
ADHD symptoms are more common in children with trans identities.
In an analysis of cross-sectional data from the Adolescent Brain Cognitive Development Study1, covering 10,227 children, children who answered “yes” or “maybe” to the question “are you transgender?” were more likely to show ADHD symptoms than those who answered “no.”
- Elizaveta Ignatova, Priyadharshini Balasubramanian, Julia H. Raney, Kyle T. Ganson, Alexander Testa, Jinbo He, Fiona C. Baker, Jason M. Nagata,
Transgender Identity and Attention Deficit Hyperactivity Disorder Symptoms: Findings From the Adolescent Brain Cognitive Development Study, Journal of Adolescent Health,
Volume 76, Issue 3, 2025. https://doi.org/10.1016/j.jadohealth.2024.10.015. ↩︎
- Elizaveta Ignatova, Priyadharshini Balasubramanian, Julia H. Raney, Kyle T. Ganson, Alexander Testa, Jinbo He, Fiona C. Baker, Jason M. Nagata,
-
Autistic traits are more common in trans-identified girls than trans-identified boys.
A cohort study of Australian children with trans identities1 found that 74.5% of the autistic group were female, compared to 64% of the non-autistic group. Females formed a significant majority of both groups.

- A comparison of gender diversity in transgender young people with and without autistic traits from the Trans 20 cohort study
Tollit, Michelle A. et al.
The Lancet Regional Health – Western Pacific, Volume 47, 101084 ↩︎
- A comparison of gender diversity in transgender young people with and without autistic traits from the Trans 20 cohort study
-
Autistic children with gender dysphoria were also more likely to be dissatisfied with other parts of their bodies.
A cohort study of Australian children with trans identities1 found that children with autistic traits were more likely to express dissatisfaction with body parts unrelated to sex (e.g. nose, feet.) The study also found that frequency of voice dysphoria was higher in the autistic trait group.
- A comparison of gender diversity in transgender young people with and without autistic traits from the Trans 20 cohort study
Tollit, Michelle A. et al.
The Lancet Regional Health – Western Pacific, Volume 47, 101084
↩︎
- A comparison of gender diversity in transgender young people with and without autistic traits from the Trans 20 cohort study
-
Rates of gender-affirming surgeries in the US tripled from 2016-2019.
A cohort study1 of data from the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample showed that 48019 patients in the US received some kind of “gender-affirming” surgery between 2016 and 2020. Numbers peaked at 13011 in 2019 then fell slightly to 12818 in 2020. The study’s authors attribute this decline to the impact of the COVID-19 pandemic though, meaning the historical peak may not have been reached by then. 7.7% of all patients (3678 of the total) were aged 12-18 at the time of their surgery. 405 of these surgeries on minors (2.4% of the whole study) were genital surgeries. More than half (52.3%, or 25099 patients) were aged 19-30.
- Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Network Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348 ↩︎
-
A systematic review demonstrated flaws in measurement of regret rates across all studies.
A systematic review of regret rates across 27 studies1 showed that every study had insufficient follow-up time and/or high drop-out rates, which seriously compromise the reliability of the data on regret rates. The review’s authors describe this as a “moderate to high” risk of bias. They also note that definitions of regret and methods of measuring it are variable, and that participants may feel shame or fear of judgement and so conceal their regret. These factors combine to make the regret rate reported in the study unreliable.
- Bustos VP, Bustos SS, Mascaro A, Del Corral G, Forte AJ, Ciudad P, Kim EA, Langstein HN, Manrique OJ. Regret after Gender-affirmation Surgery: A Systematic Review and Meta-analysis of Prevalence. Plastic and Reconstruction Surgery Global Open. 2021 Mar 19;9(3):e3477. doi: 10.1097/GOX.0000000000003477. Erratum in: Plast Reconstr Surg Glob Open. 2022 Apr 28;10(4):e4340. doi: 10.1097/GOX.0000000000004340. PMID: 33968550; PMCID: PMC8099405. ↩︎
-
High drop-out rates mean reported detransition rates are misleading.
An ethics-focused meta-study of psychosocial outcomes of “gender reassigment”1 found that 20-60% of participants were lost to follow up. Remaining research participants were more likely to report satisfaction with interventions, so reported rates of regret/desistance/detransition in such studies may be highly misleading.

- D’Angelo R. Psychiatry’s ethical involvement in gender-affirming care. Australasian Psychiatry. 2018 Oct;26(5):460-463. doi: 10.1177/1039856218775216. Epub 2018 May 21. PMID: 29783857.
↩︎
- D’Angelo R. Psychiatry’s ethical involvement in gender-affirming care. Australasian Psychiatry. 2018 Oct;26(5):460-463. doi: 10.1177/1039856218775216. Epub 2018 May 21. PMID: 29783857.
-
Time until treatment regret emerges may be eight years or more.
An analysis1 showed that the median time to surgical regret may be as high as eight years. For cross-sex hormone treatment, the time to regret may be almost eleven years (130 months). However, the analysis points out that the lack of thorough follow up in much of the research in this field, and the lack of detailed research into the detransitioner/desister population, mean that accurate figures are very hard to discern.

- Cohn, J. The Detransition Rate Is Unknown. Archives of Sexual Behaviour 52, 1937–1952 (2023). https://doi.org/10.1007/s10508-023-02623-5 ↩︎
-
Quality Of Life scores start to decline around one year after “gender-affirming” surgery. After five years, these scores are below pre-surgery levels.
A systematic review and meta-analysis1 of studies on the Quality Of Life (QoL) of transgender patients showed that in every domain, these patients tended to have poor QoL compared to the general population. Some patients showed an increase in QoL in some domains, but this peaked after about a year. After five years, these scores were below pre-transition levels.
- Nobili, A., Glazebrook, C. & Arcelus, J. Quality of life of treatment-seeking transgender adults: A systematic review and meta-analysis. Rev Endocr Metab Disord 19, 199–220 (2018). https://doi.org/10.1007/s11154-018-9459-y ↩︎
-
Cross-sex hormone treatment is stopped within four years by up to a third of patients.
In a study1 of the medical and pharmaceutical records of spouses and children of American military personnel, only 70.2% of those who started cross-sex hormone treatment continued the treatment after four years. Rates were lower for females taking male hormones (64.4%) than for males taking female hormones (81.0%).
- Christina M Roberts, David A Klein, Terry A Adirim, Natasha A Schvey, Elizabeth Hisle-Gorman, Continuation of Gender-affirming Hormones Among Transgender Adolescents and Adults, The Journal of Clinical Endocrinology & Metabolism, Volume 107, Issue 9, September 2022, Pages e3937–e3943, https://doi.org/10.1210/clinem/dgac251 ↩︎
-
36% of patients at Amsterdam gender clinic were lost to follow up.
In a study of all patients at a clinic treating 95% of all trans-identified people in the Netherlands1, 36% of all patients were lost to follow up. This may make reported rates of regret or detransition highly unreliable2. Rates of “regret” in the study itself may be compromised by a definition of “true regret” marked by beginning hormone therapy reflecting the patient’s sex (e.g. testosterone therapy for detransitioning “trans women” or estrogen therapy for detransitioning “trans men.”) The study also notes that some of those experiencing “true regret” had thought that transition would be a “solution” for their homosexuality. Regret was expressed between 46 and 271 months after beginning cross-sex hormone treatment. This may suggest there is a long tail of such regret still to come, even from those who began treatment more than twenty years ago.

- Wiepjes CM, Nota NM, de Blok CJM, Klaver M, de Vries ALC, Wensing-Kruger SA, de Jongh RT, Bouman MB, Steensma TD, Cohen-Kettenis P, Gooren LJG, Kreukels BPC, den Heijer M. The Amsterdam Cohort of Gender Dysphoria Study (1972-2015): Trends in Prevalence, Treatment, and Regrets. J Sex Med. 2018 Apr;15(4):582-590. doi: 10.1016/j.jsxm.2018.01.016. Epub 2018 Feb 17. PMID: 29463477 ↩︎
- https://catalogofbias.org/biases/attrition-bias/ ↩︎
-
Testosterone induces distinct cellular changes in female reproductive organs—including prostate-like tissue in the vagina, uterine atrophy, cyst-filled ovaries, and male-pattern cells in the cervix.
A 2025 study1 retrospectively reviewed histopathology slides from 20 trans-identifying females (ages 16–35) who underwent “gender-affirming” gynecologic surgery following 4–63 months of testosterone therapy (mean duration 21.7 ± 17.8 months).
Key findings included:
- 100% showed NKX3.1-positive basal keratinocytes in the cervix (a marker normally found in male prostate tissue)
- 55% and 60% of cervical samples showed transitional and prostatic-type metaplasia (cell changes resembling male urethral and prostate tissue)
- 100% and 50% of vaginal samples showed the same respective patterns
- 75% had an inactive uterine lining (endometrium)
- 55% showed ciliated cell metaplasia (development of hair-like cells typically not present)
- 65% had stromal expansion and decidua-like change (tissue patterns resembling early pregnancy)
- 70% had numerous cystic follicles in the ovaries, and 60% showed signs of follicular maturation
- One patient had ovarian endometriosis; one had a mucinous cyst adenofibroma
- Fallopian tubes had paratubal mesonephric remnants, but no hypertrophy (enlargement)
A comparison group of 25 benign hysterectomy samples from females of reproductive age showed no transitional or prostatic-type metaplasia, and only 2 cases (8%) had focal NKX3.1 positivity.
- Bakshi, N., Nanda, B., Rao, S., Badwal, S., & Dhawan, S. (2025). Spectrum of Histopathologic Findings in Transgender Men Undergoing Gender-Affirming Gynecologic Surgery Following Preoperative Androgen Therapy: A Tertiary Care Center Study. International journal of surgical pathology, 10668969251363990. Advance online publication. https://doi.org/10.1177/10668969251363990 ↩︎
-
Males on feminizing hormones face over double the risk of kidney stones.
A 2025 analysis1 of NIH medical records found that 10.3% of males on feminizing hormone therapy developed kidney stones, compared to 4.8% of those not on hormones. The risk was especially elevated for those on both estrogen and antiandrogens, with odds more than 2.5 times higher.
- Frangopoulos, E., Savin, Z., Gupta, K., Durbhakula, V., Gallante, B., Atallah, W. M., & Gupta, M. (2025). Increased Risk of Kidney Stones in Transgender Women and Gender-Diverse Adults on Gender-Affirming Hormone Therapy: Insights from a Large Database Study. Journal of Endourology. ↩︎
-
One in five vaginoplasty patients develop genital prolapse.
A 2025 Swiss follow‑up study1 (mean 27.5 years post‑surgery) found prolapse rates highest among those with peritoneal vaginoplasty (83%), followed by penile‑inversion techniques (17%) and intestinal vaginoplasty (14%). Surgical repairs often reduced symptoms but highlight long‑term complications rarely discussed before transition.
- Osswald, R., Villiger, A. S., Ruggeri, G., Hoehn, D., Mueller, M., & Kuhn, A. (2025). Twenty-Seven Years After Sex Reassignment Surgery in Female Transgender Patients: Is Prolapse of the Neovagina an Issue?. International Urogynecology Journal, 1-7. [Link] ↩︎
-
“Gender-affirming” hormone therapy increases BMI.
A 2025 systematic review and meta-analysis1 of 29 studies (28 included in meta-analysis) involving 2,674 individuals found that “gender-affirming” hormone therapy led to statistically significant body mass index (BMI) increases. The mean age across studies ranged from 16 to 56 years, and no prior puberty suppression was reported before the initiation of GAHT. The researchers excluded studies with adolescent samples or with pubertal suppression prior to hormone therapy. Natal males receiving feminizing hormones experienced an average BMI increase of 0.55 kg/m², while natal females receiving masculinizing testosterone showed a larger average increase of 0.92 kg/m². The study authors noted these represent modest weight gains with moderate certainty of evidence, though they concluded the changes reflect expected hormonal effects rather than pathological outcomes.
- Gois, Í., Rodrigues, F. B., Pereira, M., Dias-da-Silva, M. R., & Gomes, S. M. (2025). Body mass index and body composition changes in transgender people undergoing gender-affirming hormone therapy: a systematic review and meta-analysis. Reviews in Endocrine and Metabolic Disorders, 1-17. [Link] ↩︎
-
One study found adults diagnosed with gender incongruence were nearly four times more likely to receive antidepressants or anti-anxiety medications than the general population.
An analysis1 of the 2005−2015 Swedish Total Population and Prescribed Drug Registers examined 2,679 adults diagnosed with gender incongruence. Compared to the general population, these individuals were 3.95 times more likely to receive antidepressant prescriptions and 3.43 times more likely to receive anxiolytic (anti-anxiety) prescriptions. The study also found they were six times more likely to have mood or anxiety disorder healthcare visits and more than six times more likely to be hospitalised following suicide attempts.
- Bränström, R., & Pachankis, J. E. (2020). “Reduction in mental health treatment utilization among transgender individuals after gender-affirming surgeries: A total population study”: Correction. The American Journal of Psychiatry, 177(8), 734. https://doi.org/10.1176/appi.ajp.2019.19010080 ↩︎
-
Trans-identified adolescents are prescribed psychotropic medications more than twice as often as their siblings, with rates increasing after medical transition.
A 2021 study in the Journal of Sexual Medicine1 found that trans-identified adolescents in the US military healthcare system were prescribed psychotropic medications (such as antidepressants, sleep aids, antipsychotics, and mood stabilizers) at more than double the rate of their siblings (IRR = 2.57), with prescriptions increasing after “gender-affirming pharmaceutical initiation” (IRR = 1.67). The study compared mental health diagnoses, service use, and medication patterns before and after this medical transition step.
- Hisle-Gorman, E., Schvey, N. A., Adirim, T. A., Rayne, A. K., Susi, A., Roberts, T. A., & Klein, D. A. (2021). Mental healthcare utilization of transgender youth before and after affirming treatment. The Journal of Sexual Medicine, 18(8), 1444-1454. [Link] ↩︎
-
More than a third of UK residents in a survey did not know that “transgender women” are male.
More than a third of UK residents in a 2023 survey1 by Murray Blackburn Mackenzie—a Scottish independent policy analysis collective—did not know that “transgender women” are natal males. The findings show significant misunderstanding of the term and emphasize the need for clearer language in policy and media communication.
- Murray Blackburn Mackenzie. (2023, August 7). Clarity matters: How placating lobbyists obscures public understanding of sex and gender. Murray Blackburn Mackenzie. [Link] ↩︎
-
Around 25–50% of transmen and 5–10% of transwomen have had genital surgery.
Based on a 2019 review, genital surgery1 as part of medical transition is generally less common than chest surgery, with reported rates of 25–50% for transmen (natal females) and 5–10% for transwomen (natal males). These estimates come from a range of surveys and clinical reports.
- Nolan, I. T., Kuhner, C. J., & Dy, G. W. (2019). Demographic and temporal trends in transgender identities and gender confirming surgery. Translational andrology and urology, 8(3), 184. [Link] ↩︎
-
“Gender-affirming” surgery is associated with increased risk of depression, anxiety, suicidal ideation, and substance use disorders.
A 2025 U.S. national database study1 examined over 107,000 adults diagnosed with gender dysphoria to compare those who did and did not undergo “gender-affirming” surgery. Using matched cohorts controlling for age, race, and ethnicity, the study found significantly higher risks of depression, anxiety, suicidal ideation, and substance use disorders within two years after surgery.
For males who had surgery, depression was 25.4% vs. 11.5% without surgery (RR 2.20) and anxiety 12.8% vs. 2.6% (RR 4.88). Females also showed increased rates: depression 22.9% vs. 14.6% (RR 1.56) and anxiety 10.5% vs. 7.1% (RR 1.48). Those undergoing feminizing procedures had particularly elevated risk for depression (RR 1.78) and substance use disorders (RR 1.28).
- Lewis, J. E., Patterson, A. R., Effirim, M. A., Patel, M. M., Lim, S. E., Cuello, V. A., … & Lee, W. C. (2025). Examining gender-specific mental health risks after gender-affirming surgery: a national database study. The Journal of Sexual Medicine, 22(4), 645-651. [Link] ↩︎
-
Boys show a clear athletic advantage over girls even before puberty.
Performance data from Little Athletics Australia1 reveals that boys outperform girls in every track and field event from under-9 to under-15 age groups, even prior to puberty. This challenges the common claim that pre-pubertal boys or those on puberty blockers have no competitive edge over girls. The male performance advantage appears early in childhood and is evident across sprinting, jumping, and throwing events.
- Little Athletics Australia. (2018). Australian best performances as at August 2018 [PDF]. https://www.littleathletics.com.au/wp-content/uploads/2019/03/ABP-as-at-August-2018-V1.pdf
↩︎
- Little Athletics Australia. (2018). Australian best performances as at August 2018 [PDF]. https://www.littleathletics.com.au/wp-content/uploads/2019/03/ABP-as-at-August-2018-V1.pdf
-
A Finnish study found detransitioners commonly had psychiatric comorbidities and childhood trauma, with most concluding their gender dysphoria arose from psychological distress rather than transgender identity.
A 2025 case series1 from Helsinki University Hospital reviewed nine adults who sought medical detransition after previously receiving “gender-affirming” treatments.
Seven were natal females and all expressed “major regret”; both natal males expressed “minor regret.” The average time from diagnosis to regret was 7 years. Patients had used hormones for an average of 7 years (median 4 years), with eight undergoing chest reconstruction/augmentation surgery and four females having reproductive organs surgically removed.
All nine had psychiatric comorbidities—mood disorders were most common (8 patients: 2 with bipolar II, 6 with depression), anxiety disorders (6 patients initially, 7 by detransition), personality disorders (3 patients, with borderline personality disorder increasing from 2 to 5 patients by detransition), and dissociative disorders (1 initially, 3 total). Childhood trauma was universal, with all having insecure attachment styles. Six reported sexual abuse/rape and six experienced school bullying. Eating disorders were diagnosed in 4 patients, with 78% having eating disorder symptoms.
Patients retrospectively believed their gender dysphoria stemmed from unresolved psychological stressors and developmental challenges rather than a stable transgender identity. The clinic has since revised its protocols to improve psychiatric screening, facilitate easier re-access for detransitioners without referrals, and emphasize clinical neutrality.
- Kettula, K., Puustinen, N., Tynkkynen, L., Lempinen, L., & Tuisku, K. (2025). Gender Dysphoria and Detransitioning in Adults: An Analysis of Nine Patients from a Gender Identity Clinic from Finland. Archives of Sexual Behavior, 54(5), 1981-1990. [Link] ↩︎
-
Estrogen use in trans-identified males is associated with a wide range of serious health risks—including blood clots, stroke, cancer, infertility, and cognitive decline.
A 2025 review1 summarizes wide-ranging risks tied to estrogen use in trans-identified males:
- 2.2× higher risk of blood clots (VTE)
- Up to 10× higher risk of stroke after 6 years on estrogen
- 1.8× higher all-cause mortality compared to other males
- 22.5–40.7× higher risk of breast cancer vs. male baseline
- 3× higher risk of cardiovascular death with estradiol use
- 72% increase in insulin resistance after 1 year; additional 9% in year 2
- Reduced brain volume and slower processing speed with long-term use
- Cognitive decline and elevated depression markers over time
- Only 0–24% retain sperm production after starting estrogen
- 6.6× higher incidence of multiple sclerosis
- Case reports of pancreatitis, autoimmune flare-ups, and brain tumors (meningioma)
The review emphasizes that many of these risks are under-recognized in clinical practice, raising urgent concerns about safety and informed consent.
- Schwartz, L., Lal, M., Cohn, J., Mendoza, C. D., & MacMillan, L. (2025). Emerging and accumulating safety signals for the use of estrogen among transgender women. Discover Mental Health, 5(1), 1-17. [Link] ↩︎
-
Testosterone therapy is associated with nearly doubled depression risk and 52% higher suicide attempt rates in men within five years.
In a 2022 study1 published in the Journal of Sexual Medicine, researchers analyzed 70.3 million electronic health records from 46 healthcare organizations to examine mental health outcomes in men using testosterone therapy. The study compared 263,579 men who used testosterone to over 17.8 million men who did not. Results showed testosterone use was independently associated with a 99% increased risk of major depressive disorder (OR 1.99, 95% CI 1.94-2.04) and a 52% increased risk of suicide attempts or intentional self-harm (OR 1.52, 95% CI 1.40-1.65) within 5 years of use. These associations remained significant even when analyzing only men with clinically diagnosed testosterone deficiency, suggesting the mental health risks persist regardless of baseline testosterone levels.
- Nackeeran, S., Patel, M. S., Nallakumar, D. T., Ory, J., Kohn, T., Deibert, C. M., Carto, C., & Ramasamy, R. (2022). Testosterone Therapy is Associated With Depression, Suicidality, and Intentional Self-Harm: Analysis of a National Federated Database. Journal of Sexual Medicine, 19(6), 933-939. PMID: 35437187. [Link] ↩︎
-
Testosterone use in females triggers biological signs of kidney stress and injury within just three months.
In a 2025 study in the Journal of Clinical Investigation1, females taking testosterone for gender transition showed biological changes consistent with subclinical kidney stress and tubular injury after three months—including a 134% increase in a urinary marker linked to kidney inflammation (YKL-40) and an 8% rise in an inflammatory blood protein (TNF receptor-1). Although overall kidney filtration remained unchanged, testosterone negatively affected kidney-protective proteins and activated pathways tied to inflammation, tissue remodeling, and fibrosis. The researchers called for long-term studies in larger populations to assess potential lasting effects.
- van Eeghen, S. A., Pyle, L., Narongkiatikhun, P., Choi, Y. J., Obeid, W., Parikh, C. R., … & Nokoff, N. J. (2025). Unveiling mechanisms underlying kidney function changes during sex hormone therapy. The Journal of Clinical Investigation. [Link]
↩︎
- van Eeghen, S. A., Pyle, L., Narongkiatikhun, P., Choi, Y. J., Obeid, W., Parikh, C. R., … & Nokoff, N. J. (2025). Unveiling mechanisms underlying kidney function changes during sex hormone therapy. The Journal of Clinical Investigation. [Link]
-
Trans-identified females report higher rates of sexual assault than their male counterparts.
A study by Abern et al.1 surveyed 996 trans-identified adults and found that 50% of females reported experiencing sexual assault, compared to 37% of males.
- Abern, L., Diego, D., Krempasky, C., Cook, J., & Maguire, K. (2023). Prevalence of sexual assault in a cohort of transgender and gender diverse individuals. Journal of general internal medicine, 38(5), 1331-1333. [Link] ↩︎
-
Genital surgery is associated with high rates of pelvic floor and sexual dysfunction.
A 2025 systematic review and meta-analysis1 examined 25 studies on pelvic floor outcomes after genital “gender-affirming” surgery. The findings show a high prevalence of complications among both male and female patients:
Type of Dysfunction Males (vaginoplasty) Females (hysterectomy & phalloplasty) Pelvic organ prolapse 1–7.5% 3.8% Urinary incontinence up to 15% up to 50% Urinary irritative symptoms up to 20% up to 37% Sexual dysfunction 25–75% 54% - Dominoni, M., Scatigno, A. L., Pasquali, M. F., Bergante, C., Gariboldi, F., & Gardella, B. (2025). Pelvic floor and sexual dysfunctions after genital gender-affirming surgery: a systematic review and meta-analysis. The Journal of Sexual Medicine, 22(1), 184-195. [Link] ↩︎
-
Polycystic ovary syndrome (PCOS) is more prevalent in females seeking medical transition.
A 2025 study1 from Argentina found that 26.6% of female adults presenting for “gender-affirming hormone therapy” had polycystic ovary syndrome (PCOS) prior to starting any hormonal treatment. PCOS is a hormonal disorder characterized by irregular periods, excess male hormone levels, and cysts on the ovaries. This rate is 2-3 times higher than the 8-13% prevalence in the general female population.2
A 2024 study3 from the Cleveland Clinic similarly found 23.8% of adolescent females presenting for “gender-affirming hormone therapy” had PCOS, with higher male hormone levels, higher BMIs, and increased rates of dyslipidemia than those without PCOS.
- Calvar, C. E., Di Noto, M., Lema Villacis, M., Blanco Hirota, N., & Anticona Sayán, M. I. (2025). Prevalencia, distribución fenotípica y riesgo cardiometabólico del síndrome de ovario poliquístico en población transgénero [Prevalence, phenotype distribution and cardiometabolic risk of polycystic ovarian syndrome in transgender population]. Medicina, 85(1), 31–38. [Link] ↩︎
- March, W. A., Moore, V. M., Willson, K. J., Phillips, D. I., Norman, R. J., & Davies, M. J. (2010). The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Human reproduction, 25(2), 544-551. [Link]
↩︎ - Rangi, S. K., Rehmer, J., & Ferrando, C. A. (2024). Prevalence of polycystic ovarian syndrome in young and adolescent transmasculine patients presenting for gender-affirming care. Journal of Pediatric and Adolescent Gynecology, 37(1), 51-55. [Link] ↩︎
-
Puberty blockers potentially have a negative impact on neuropsychological functioning
A 2024 review by Sallie Baxendale1 extensively examined the neuropsychological impacts of puberty blockers. The review indicated that animal studies showed a non-reversible negative impact on cognitive and behavioral functions. In human studies, the evidence suggested detrimental effects on IQ among those treated with puberty blockers for precocious puberty. Specifically, one study documented an average decrease in full-scale IQ of 7 points, including a case where an individual’s IQ fell by 15 points from 138 to 123 after treatment. Another case study involving a gender dysphoric young person reported a drop of 9 points in global (overall) IQ and 15 points in working memory during the course of treatment with puberty blockers.
- Baxendale, S. (2024). The impact of suppressing puberty on neuropsychological function: A review. Acta Paediatrica, 113(7), 1156-1167. [Link] ↩︎
-
People who have undergone cross-sex surgery are over 19 times more likely to die by suicide than the general population
Dhejne et al. (2011)1 conducted the longest follow-up study to date on the outcomes of “sex reassignment surgery”, covering a period of 30 years (1973-2003) and involving 324 individuals in Sweden. The study compared these individuals to matched controls based on birth year and sex, revealing that those who had undergone surgery exhibited a significantly increased suicide risk, with rates nearly 19.1 times higher than their matched controls.
- Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L., Långström, N., & Landén, M. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PloS one, 6(2), e16885. [Link] ↩︎
-
Long-term testosterone use in females may induce early menopause, leading to pelvic dysfunction, increased mortality risk and many other challenges
A 2024 study by da Silva et al1. found that 94.1% of 68 trans-identified females using testosterone experienced pelvic dysfunctions typically seen in postmenopausal women, including urinary (86.7%), sexual (52.9%), and bowel (45.6%) problems. These symptoms appeared as early as age 18, with an average onset age of 28.
This early onset of menopausal-like symptoms is particularly concerning given findings from another 2024 study by Haapakoski et al.2, which demonstrated increased mortality risks associated with early menopause. The study found that women experiencing early menopause (n=5,800) were twice as likely to die from heart disease and four times more likely to die from cancer compared to those with typical menopause onset (n=23,000).
Testosterone use may induce early menopause by inhibiting ovarian function3 and decreasing estrogen production in the body4.
- da Silva, L. M. B., Freire, S. N. D., Moretti, E., & Barbosa, L. (2024). Pelvic Floor Dysfunction in Transgender Men on Gender-affirming Hormone Therapy: A Descriptive Cross-sectional Study. International Urogynecology Journal, 1-8. [Link] ↩︎
- Haapakoski, H., Silven, H., Pesonen, P., Savukoski, S., & Niinimaki, M. (2024, May). Mortality among women with POI, nationwide register based case-control study. In Endocrine Abstracts (Vol. 99). Bioscientifica. [Link] ↩︎
- Bailie, E., Maidarti, M., Hawthorn, R., Jack, S., Watson, N., Telfer, E. E., & Anderson, R. A. (2023). The ovaries of transgender men indicate effects of high dose testosterone on the primordial and early growing follicle pool. Reproduction and Fertility, 4(2). [Link] ↩︎
- Chan, K. J., Jolly, D., Liang, J. J., Weinand, J. D., & Safer, J. D. (2018). Estrogen levels do not rise with testosterone treatment for transgender men. Endocrine Practice, 24(4), 329-333. [Link] ↩︎
-
Increased media coverage of “transgender and gender diverse” issues is associated with higher referral rates to pediatric gender clinics.
A 2020 study by Pang et al1. explored the impact of media coverage on the referral rates to two specific pediatric gender clinics: the Gender Identity Development Service in the UK, and the Royal Children’s Hospital Gender Service (RCHGS) in Australia. Analyzing data from over 5,000 referrals collected over an eight-year period, the study found a strong correlation between the amount of “transgender and gender diverse” media coverage and the number of referrals to these clinics. The research highlighted that an uptick in media stories led to increased referrals, with a significant spike observed one week after coverage in the UK and two weeks later in Australia.
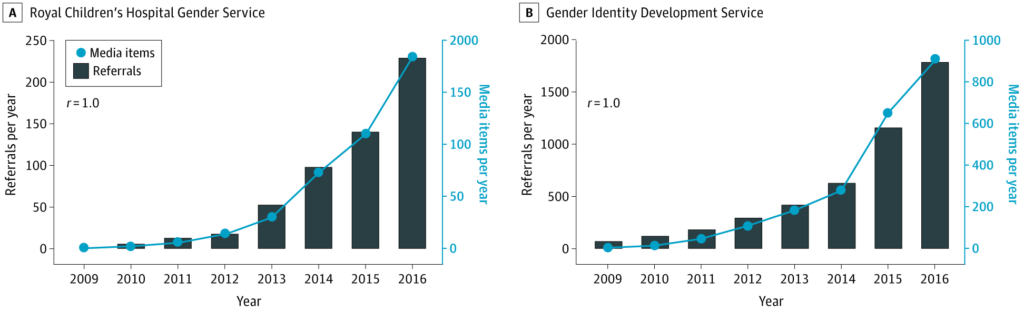
Annual Referrals to the Royal Children’s Hospital Gender Service and Gender Identity Development Service and Transgender- and Gender Diverse–Related Media Stories. - Pang, K. C., de Graaf, N. M., Chew, D., Hoq, M., Keith, D. R., Carmichael, P., & Steensma, T. D. (2020). Association of media coverage of transgender and gender diverse issues with rates of referral of transgender children and adolescents to specialist gender clinics in the UK and Australia. JAMA Network Open, 3(7), e2011161-e2011161. [Link] ↩︎
-
Trans-identified and gender-questioning adolescents engage in significantly more recreational screen time and exhibit higher rates of problematic screen use compared to their peers
Using data from the third year of the U.S. Adolescent Brain Cognitive Development Study, which included 9,859 participants mostly aged 12-13, Nagata et al. (2024)1 found that trans-identified youth report an average of 4.51 more hours of daily screen time, and gender-questioning youth report 3.41 more hours, compared to other youth. This screen time includes activities such as browsing the internet, playing video games, texting, using social media, and watching television and movies. Adjusting for various confounders, the study also indicated higher instances of problematic use of social media, video games, and mobile phones among these groups. Problematic use was defined as being “characterized by inability to control usage and detrimental consequences from excessive use including preoccupation, tolerance, relapse, withdrawal, and conflict.”
- Nagata, J. M., Balasubramanian, P., Iyra, P., Ganson, K. T., Testa, A., He, J., … & Baker, F. C. (2024). Screen use in transgender and gender-questioning adolescents: Findings from the Adolescent Brain Cognitive Development (ABCD) Study. Annals of Epidemiology, 95, 6-11. [Link] ↩︎
-
People who have undergone cross-sex surgery exhibit a significantly higher suicide risk
Dhejne et al. (2011)1 conducted the longest follow-up study to date on the outcomes of “sex reassignment surgery”, covering a period of 30 years (1973-2003) and involving 324 individuals in Sweden. The study compared these individuals to matched controls based on birth year and sex, revealing that those who had undergone surgery exhibited a significantly increased suicide risk, with rates nearly 19.1 times higher than their matched controls.
In the US, a 2024 study by Straub et al.2 analyzed the psychiatric risks of those who’ve undergone “gender-affirmation surgery” using a large patient dataset. This study compared individuals who had undergone the surgery to two control groups: one consisting of adults who had emergency department visits without any surgery and another comprising individuals who underwent either a tubal ligation or vasectomy. The findings indicated that those who had “gender-affirmation surgery” faced a 12.12-fold increased risk of attempting suicide compared to the emergency visit control group, and a 4.71-fold higher risk compared to the tubal ligation/vasectomy control group.
- Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L., Långström, N., & Landén, M. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PloS one, 6(2), e16885. [Link] ↩︎
- Straub, J. J., Paul, K. K., Bothwell, L. G., Deshazo, S. J., Golovko, G., Miller, M. S., & Jehle, D. V. (2024). Risk of suicide and self-harm following gender-affirmation surgery. Cureus, 16(4). [Link] ↩︎
-
There is no high-quality evidence supporting the use of puberty blockers for gender distress
A 2024 systematic review by Taylor et al. at the University of York1 was commissioned by the Cass Review to rigorously assess the safety and effectiveness of puberty suppression in adolescents with gender dysphoria. Analyzing studies up to April 2022, the review included 11 cohort, 8 cross-sectional, and 31 pre-post studies, but only one cross-sectional study met high-quality standards. The meta-analysis of moderate to high-quality studies showed limited and inconsistent evidence of benefits in areas like gender dysphoria, mental health, and body satisfaction.
This finding aligns with the previous 2020 review by the British National Institute for Clinical Excellence (NICE) on puberty blockers2, which described the supporting evidence as “very low” quality. The review noted minimal changes in key outcomes like gender dysphoria, mental health, and quality of life due to small, uncontrolled observational studies. Furthermore, a 2024 review from Germany by Zepf et al.3, adhering to NICE criteria, confirmed the absence of new studies on puberty blockers for gender dysphoria since the NICE review.
- Taylor, J., Mitchell, A., Hall, R., Heathcote, C., Langton, T., Fraser, L., & Hewitt, C. E. (2024). Interventions to suppress puberty in adolescents experiencing gender dysphoria or incongruence: a systematic review. Archives of disease in childhood, archdischild-2023-326669. [Link] ↩︎
- National Institute for Health and Care Excellence (2021). Evidence review: Gonadotrophin releasing hormone analogues for children and adolescents with gender dysphoria. National Institute for Health and Care Excellence (NICE); NHS England; NHS Improvement. [Link] ↩︎
- Zepf, F. D., König, L., Kaiser, A., Ligges, C., Ligges, M., Roessner, V., … & Holtmann, M. (2024). Beyond NICE: Aktualisierte systematische Übersicht zur Evidenzlage der Pubertätsblockade und Hormongabe bei Minderjährigen mit Geschlechtsdysphorie. Zeitschrift für Kinder-und Jugendpsychiatrie und Psychotherapie. [Link] ↩︎
-
Autism and gender dysphoria occur together at significantly high rates.
The connection between autism and gender dysphoria has emerged through increasingly robust research over the past decade. Early systematic reviews (Glidden et al., 2016)1 first identified unexpectedly high autism rates among youth with gender dysphoria diagnoses.
Clinical studies then provided stronger evidence. Hisle-Gorman et al. (2019)2 found children with autism diagnoses were over four times more likely to receive a gender dysphoria diagnosis. Warrier et al. (2020)3 confirmed elevated rates across five large independent datasets.
Kallitsounaki & Williams’ 2023 meta-analysis4 synthesized 47 studies – including the ones above – finding that 11% of individuals with gender dysphoria have autism diagnoses—compared to 1% in the general population. The analysis also showed statistically significant differences in autism traits between those with gender dysphoria and control groups (g=0.67), with the authors noting the rising number of publications on this overlap.
Kahn et al.’s 2023 study5 analyzed 919,898 youth across eight U.S. hospital systems, revealing that 0.05% had diagnoses of both autism and gender dysphoria. The probability of having a gender dysphoria diagnosis was 0.019 for those with autism, compared to 0.006 for those without—representing three times higher odds (aOR=3.00).
- Glidden, D., Bouman, W. P., Jones, B. A., & Arcelus, J. (2016). Gender dysphoria and autism spectrum disorder: A systematic review of the literature. Sexual Medicine Reviews, 4(1), 3–14. ↩︎
- Hisle-Gorman, E., Landis, C. A., Susi, A., Schvey, N. A., Gorman, G. H., Nylund, C. M., & Klein, D. A. (2019). Gender dysphoria in children with autism spectrum disorder. LGBT Health, 6(3), 95–100. ↩︎
- Warrier, V., Greenberg, D. M., Weir, E., Buckingham, C., Smith, P., Lai, M. C., … & Baron-Cohen, S. (2020). Elevated rates of autism, other neurodevelopmental and psychiatric diagnoses, and autistic traits in transgender and gender-diverse individuals. Nature Communications, 11(1), 3959. ↩︎
- Kallitsounaki, A., & Williams, D. M. (2023). Autism spectrum disorder and gender dysphoria/incongruence: A systematic literature review and meta-analysis. Journal of Autism and Developmental Disorders, 53(8), 3103–3117. ↩︎
- Kahn, N. F., Sequeira, G. M., Garrison, M. M., Orlich, F., Christakis, D. A., Aye, T., … & Richardson, L. P. (2023). Co-occurring autism spectrum disorder and gender dysphoria in adolescents. Pediatrics, 152(2), e2023061363. ↩︎
-
Female world-class athletes largely view the inclusion of trans-identified males in female sport categories as unfair, particularly in sports that emphasize physical capacity
Among female world-class athletes, 77% opposed the inclusion of trans-identified males in female categories, citing significant fairness concerns. This opposition was especially pronounced in sports relying heavily on physical capacity, such as track and field and weightlifting. Precision sports like archery saw much lower levels of concern, with only 35.7% of athletes viewing the inclusion as unfair
Shaw et. al (2024)1 surveyed female 175 athletes, stratified into three competitive levels based on proximity to world records and level of competition: 26 world-class (Tier 5) athletes, including Olympic or World Championship finalists or those within 2% of world records; 49 elite (Tier 4) athletes, who have competed internationally or are within 7% of world records; and 100 national level (Tier 3) athletes, who have competed nationally or are within 20% of world records. Overall, 58% of these athletes supported categorizing sports based on biological sex.
- Shaw, A. L., Williams, A. G., Stebbings, G. K., Chollier, M., Harvey, A., & Heffernan, S. M. (2024). The perspective of current and retired world class, elite and national athletes on the inclusion and eligibility of transgender athletes in elite sport. Journal of Sports Sciences, 42(5), 381-391. [Link] ↩︎
-
Intestinal vaginoplasty in patients with stunted penile growth from puberty blockers can lead to bowel inflammation, excessive discharge, persistent foul odors, and fecal leakage
A 2017 survey by Milrod and Karasic1 found WPATH-affiliated surgeons in the United States considered sigmoid- or ileum-derived vaginoplasty (using sections of large or small intestine) an option for patients who had used puberty blockers. These patients, who had sometimes used blockers for up to 3 years, had severely underdeveloped genitals, described as “11-year-old genitalia” or a “micropenis,” which complicated standard surgical techniques. However, this intestinal approach was associated with serious complications, including diversion colitis (inflammation of the repurposed bowel tissue), excessive secretion, persistent foul odors, and potential leakage of stool into the peritoneum (the membrane lining the abdominal cavity).
- Milrod, C., & Karasic, D. H. (2017). Age is just a number: WPATH-affiliated surgeons’ experiences and attitudes toward vaginoplasty in transgender females under 18 years of age in the United States. The Journal of Sexual Medicine, 14(4), 624-634. [Link] ↩︎
-
There is a significant burden of chronic pain in trans-identified individuals, with an increased risk among those receiving cross-sex hormones
A 2024 large US clinical database study1 of 98,352 trans-identified individuals (56,470 females and 41,882 males) found significantly higher rates of chronic pain compared to the general population. Of particular concern, those receiving cross-sex hormones showed even higher risks – females on testosterone had a 20% increased hazard of chronic pain diagnosis compared to those not taking testosterone, while males on estrogen showed a 19.4% increased risk.
- Tabernacki, T., Gilbert, D., Rhodes, S., Scarberry, K., Pope, R., McNamara, M., … & Mishra, K. (2024). The burden of chronic pain in transgender and gender diverse populations: Evidence from a large US clinical database. European Journal of Pain. [Link] ↩︎
-
Genital masculinizing surgeries rose by 424% and feminizing surgeries by 343% in Germany between 2006 and 2022
A 2024 German national study1 analyzing hospital records found that genital “gender-affirming” surgeries increased nearly 5-fold between 2006 and 2022. Masculinizing surgeries showed the most dramatic increase at 424%, with their highest annual rise occurring between 2018-2019, while feminizing surgeries increased by 343%, with their steepest rise between 2015-2016. The study found a dramatic shift toward younger patients, with over 70% of masculinizing and about half of feminizing surgeries performed on people aged 20-34 in 2022, compared to about a quarter for both types in 2006. These procedures became increasingly concentrated in specialized centers, with half of hospitals performing over 50 masculinizing surgeries annually by 2022, up from 15% in 2006.
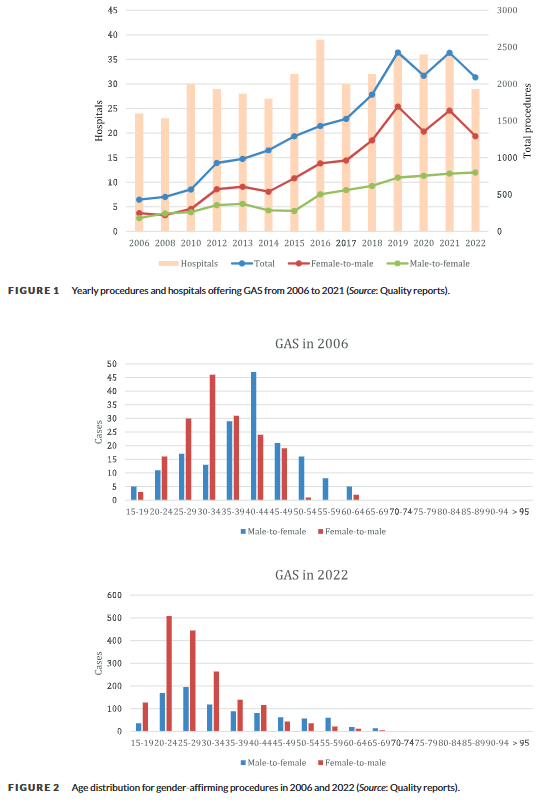
- Aksoy, C., Wellenbrock, S., Reimold, P., Karschuck, P., Ozturk, M., Hirsch, T., … & Flegar, L. (2024). Genital gender‐affirming surgery trends in Germany: Total population data with 19,600 cases from 2006 to 2022. Andrology. [Link] ↩︎
-
Suppressing sex hormones in males, using treatments like those prescribed as puberty blockers, is linked to an increased risk of dementia
A 2025 systematic review and meta-analysis1 found that men receiving androgen deprivation therapy (ADT) for prostate cancer had an increased risk of dementia, with a 26% higher likelihood for all types of dementia and a 9% higher risk specifically for Alzheimer’s disease, compared to men not receiving this treatment. ADT reduces the effects of male sex hormones (androgens) such as testosterone and dihydrotestosterone (DHT). This is achieved using medications, including GnRH agonists (which initially stimulate and then suppress hormone production via the pituitary gland), GnRH antagonists (which directly block hormone receptor activity), or through other pharmaceutical and surgical approaches. Notably, some of the same medications used for ADT—GnRH agonists, GnRH antagonists, and certain antiandrogens—are also employed as “puberty blockers” to delay puberty in children and adolescents.
- Ma, L., Tan, E. C., Goudey, B., Jin, L., & Pan, Y. (2025). Unraveling the bidirectional link between cancer and dementia and the impact of cancer therapies on dementia risk: A systematic review and meta‐analysis. Alzheimer’s & Dementia, e14540. [Link] ↩︎
-
Long term use of male sex hormones in females is deleterious to their health
The state-sponsored doping program of the German Democratic Republic (GDR) systematically administered androgens and other drugs to several thousand athletes, including minors, from 1966 onwards, leading to harmful side effects such as virilization in adolescent girls and female athletes, and other damaging effects that required medical and surgical interventions1.
Initiated in 1966, the German Democratic Republic (GDR) embarked on an extensive state-sponsored doping program. This program involved the systematic delivery of androgens and other substances to thousands of athletes, some of whom were minors. Women and adolescent girls were at the core of this program as the introduction of androgens was discovered to dramatically enhance their athletic performance. The ensuing side effects, including virilization in females, were deleterious and often so severe that they required medical and surgical responses. The program’s existence was only unveiled with the fall of the GDR in 1990, through the recovery of preserved classified documents.
- Franke, W. W., & Berendonk, B. (1997). Hormonal doping and androgenization of athletes: a secret program of the German Democratic Republic government. Clinical chemistry, 43(7), 1262-1279. [Link] ↩︎
-
Long term testosterone use potentially compromises fertility and negatively affects ovarian follicle health
One study in 2023 found that long-term testosterone exposure, as seen in transgender men undergoing gender-affirming therapy, could potentially compromise fertility by negatively affecting ovarian follicle growth, health, and DNA integrity.
In 2023, a study by Bailie et al1. explored the effects of long-term testosterone exposure on ovarian follicles in transgender men receiving gender-affirming endocrine therapy. The research indicated that testosterone was linked with decreased follicle growth activation, poor follicle health, and increased DNA damage, suggesting possible impacts on fertility. Further, these negative effects were intensified following six days of in vitro culture. These findings may have crucial implications for reproductive health and fertility considerations among transgender men receiving testosterone as part of their gender-affirming therapy.
- Bailie, E., Maidarti, M., Hawthorn, R., Jack, S., Watson, N., Telfer, E. E., & Anderson, R. A. (2023). The ovaries of transgender men indicate effects of high dose testosterone on the primordial and early growing follicle pool. Reproduction and Fertility, 4(2). [Link] ↩︎
-
Long term use of anabolic-androgenic steroids (synthetic testosterone) is associated with brain ageing and a decline in cognitive processing
One study suggests that long-term use of anabolic-androgenic steroids (AAS) may cause accelerated brain ageing in certain regions, which could lead to cognitive abnormalities.
A 2021 study by Bjørnebekk et al1. aimed to investigate the effects of long-term anabolic-androgenic steroid (AAS) use on brain ageing. The study included 229 male participants, 130 of whom were long-term AAS users and 99 were non-users. The participants underwent T1-weighted magnetic resonance imaging (MRI) scans to assess brain ageing. The results showed that long-term AAS use is associated with accentuated brain ageing in certain regions, particularly the frontal and cingulate regions. The study highlights the need for further research on the long-term effects of AAS use on brain health and cognition.
- Bjørnebekk, A., Kaufmann, T., Hauger, L. E., Klonteig, S., Hullstein, I. R., & Westlye, L. T. (2021). Long-term anabolic–androgenic steroid use is associated with deviant brain ageing. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 6(5), 579-589. [Link] ↩︎
-
60% of males and 70% of females attending the world’s largest gender clinic (GIDS) are same-sex attracted
In the 2015 statistics from GIDS, approximately 60% of the youth seen there who were biological males and 70% who were biological females reported attraction to the same sex or to both sexes1.
The 2015 Gender Identity Development Service (GIDS) statistics revealed a notably high rate of same-sex attraction among the youth seen at their clinic. Over half of the biological females reported same-sex attraction, about 20% were attracted to both sexes, and a quarter to the opposite sex, with the remaining identifying as asexual. Among biological males, approximately 30% reported same-sex attraction, another 30% to both sexes, 30% to the opposite sex, with the last 10% identifying as asexual or reporting no sexual attraction.
Download as PDF -
In one peer-reviewed study of 100 detransitioners, 76% did not inform their clinicians that they had detransitioned
The majority (55%) felt they did not receive an adequate evaluation from a doctor or mental health professional before starting their transition1.
38% believed that their gender dysphoria was caused by something specific such as trauma, abuse, or a mental health condition.
- Littman L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Archives of sexual behavior, 50(8), 3353–3369. [Link] ↩︎
-
One year of cross sex hormone therapy causes robust increases in muscle mass and strength in transmen (females) but modest changes in transwomen (males)
Thigh muscle volume increased 15% in transmen, which was paralleled by increased quadriceps cross-sectional area (CSA) (15%) and radiological density 6%. In transwomen, the corresponding parameters decreased by –5% (muscle volume) and –4% (CSA), while density remained unaltered. The transmen increased strength over the assessment period, while the transwomen generally maintained their strength levels1:

- Wiik, A., Lundberg, T. R., Rullman, E., Andersson, D. P., Holmberg, et al. (2019). Muscle strength, size, and composition following 12 months of gender-affirming treatment in transgender individuals. The Journal of Clinical Endocrinology & Metabolism, 105(3). [Link] ↩︎
-
Strength advantage over females is retained by male-to-female transitioners (transwomen)
A systematic review of 24 studies concluded that while male-female transitioners (transwomen) do experience some decrease in muscle mass; values for strength and muscle area in transwomen remain above those of biological women, even after 36 months of hormone therapy.
Figure one1:

The above graph show’s the performance difference between transwomen and biological women in various sports. A systematic review of 24 studies concluded that while male-female transitioners (trans women) do experience a decrease in muscle mass; values for strength and muscle area in transwomen remain above those of biological women, even after 36 months of hormone therapy2.
- Hilton, E. N. & Lundberg, T.R. (2021). Transgender Women in the Female Category of Sport: Perspectives on Testosterone Suppression and Performance Advantage. Sports Med 51: 199–214. [Link] ↩︎
- Harper J, O’Donnell E, Sorouri Khorashad B, et al . (2021). How does hormone transition in transgender women change body composition, muscle strength and haemoglobin? Systematic review with a focus on the implications for sport participation. British Journal of Sports Medicine ;55:865-872. [Link] ↩︎
-
The linguistic term ‘Two-Spirit’ was invented in 1990
The term ‘Two-Spirit’ – often abbreviated to ‘2S’, and particularly common in Canada – is a modern invention. It was first coined at the Indigenous Lesbian and Gay International Gathering in Winnipeg, Manitoba, in 19901.
- de Vries, K. M. (2009). Berdache (Two-Spirit). In O’Brien, J. (ed.): Encyclopedia of gender and society. Los Angeles: SAGE. [Link] ↩︎
-
It is not true that 1.7% of the population is ‘born between the sexes’. The proportion of people with DSDs (‘intersex’ conditions) is 0.018%
Conditions in which chromosomal sex is inconsistent with phenotypic sex, or in which the phenotype is not classifiable as either male or female, occur in 0.018% of the population1.
The claim that 1.7% of the population is ‘intersex’2 includes conditions which most clinicians do not recognize as intersex, and is often wrongly used to back up the ideological assertion that ‘sex is a spectrum’, or that biological sex is not dimorphic.
The philosopher Kathleen Stock points out that she would be considered as “intersex” under Fausto-Sterling’s “preposterously over-demanding conditions on sex category membership”, as she lost an ovary in early adulthood3, which would count as “intersex” according to Fausto-Sterling.
- Sax, L. (2002). How common is intersex? a response to Anne Fausto-Sterling. J Sex Res. 39 (3): 174-8. [Link] ↩︎
- Fausto-Sterling, A. (2000). Sexing the Body: Gender Politics and the Construction of Sexuality. New York: Basic Books. [Link] ↩︎
- Stock, K. (2021). Material Girls. Little, Brown Book Group: p.56 [Link] ↩︎
-
There are 2 sexes: male and female. Biological sex is not a spectrum
According to an Endocrine Society Scientific Statement1,
Sex is dichotomous, with sex determination in the fertilized zygote stemming from unequal expression of sex chromosomal genes.
Sex differences in baseline physiology and associated mechanisms form the foundation for understanding sex differences in diseases pathology, treatments, and outcomes.
The erroneous claim that biological sex is a spectrum, or non-dichotomous, is often used to justify the ideological assertion that all humans are ‘assigned sex at birth’. In fact, biological sex is encoded in every cell of the body2.
- Bhargava, A., Arnold, A.P., Bangasser, D.A., Denton, K.M., Gupta, A., Hilliard Krause, L.M., Mayer, E.A., McCarthy, M., Miller, W.L., Raznahan, A. & Verma, R. (2021). Considering Sex as a Biological Variable in Basic and Clinical Studies: An Endocrine Society Scientific Statement. Endocrine Reviews 42 (3): 219-258. [Link] ↩︎
- Shah, K. McCormack, C. & Bradbury, N. (2014). Do you know the sex of your cells?’ American Journal of Physiology – Cell Physiology, C3-C18, 306, 1. [Link] ↩︎
-
In one study of detransitioners, males were three times more likely than females to have transitioned for erotic reasons
In a study1 of 100 detransitioners, 38.7% of males identified with the comment “I had erotic reasons for wanting to transition”.
The figure for females was a third of this, at 13%.
- Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Arch Sex Behav. [Link] ↩︎
-
In one study, female detransitioners were three times more likely to be lesbians than to be straight
A study1 of 100 detransitioners, the majority of whom were female, showed that 26.1% of the females were homosexual before they transitioned.
Only 8.7% considered themselves heterosexual.
- Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Arch Sex Behav. [Link] ↩︎
-
One study of detransitioners found that a large proportion of them believed, in hindsight, that they were suffering from internalized homophobia
A study of 100 detransitioners1 found that homophobia or difficulty accepting themselves as lesbian, gay, or bisexual was expressed by 23.0% as a reason for transition and subsequent detransition.
In another study of detransitioners and desisters2 – most of whom were detransitioners who had undergone medical transition – 52% expressed a psychological need for learning to cope with internalized homophobia.
- Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Arch Sex Behav. [Link] ↩︎
- Vandenbussche, E. (2021). Detransition-Related Needs and Support: A Cross-Sectional Online Survey. Journal of Homosexuality. [Link] ↩︎
-
In one study of detransitioners, around half believed that they received inadequate care
The majority (55.0%) of detransitioners in a 100-participant study1 felt that they did not receive an adequate evaluation from a doctor or mental health professional before starting transition.
A second study2 of detransitioners and desisters – most of whom were detransitioners who had undergone medical transition – arrived at a similar, although slightly lower, figure, with 45% of detransitioners not feeling properly informed about the health implications of the accessed treatments and interventions before undergoing them.
- Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Arch Sex Behav. [Link] ↩︎
- Vandenbussche, E. (2021). Detransition-Related Needs and Support: A Cross-Sectional Online Survey. Journal of Homosexuality. [Link] ↩︎
-
In one study of detransitioners, around half were worried about the medical complications of transitioning
A study1 of 100 detransitioners showed that 49% had concerns about potential medical complications from transitioning.
A second study2 of detransitioners and desisters – most of whom were detransitioners who had undergone medical transition – arrived at a higher figure, with 62% citing health concerns as a motivating factor for detransition.
- Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Arch Sex Behav. [Link] ↩︎
- Vandenbussche, E. (2021). Detransition-Related Needs and Support: A Cross-Sectional Online Survey. Journal of Homosexuality. [Link] ↩︎
-
There is very little evidence on the number of people who have detransitioned
In a study1 of 100 detransitioners, only 24% of respondents informed their clinicians that they had detransitioned. The vast majority made no attempt to contact their clinics.
Not only does this mean that we have no way of ascertaining how many people detransition, it also potentially impact clinics’ assessments of patient satisfaction.
One paper2 claimed that the detransition rate was 13.1%. However, this research relies on data from the U.S. Transgender Survey, which was conducted via community outreach organizations, and may therefore have excluded detransitioners who were no longer in touch with any such organizations. Only people who still identified as members of the trans community were included:
The 2015 U.S. Transgender Survey (USTS) was conducted by the National Center for Transgender Equality (NCTE) to examine the experiences of transgender adults in the United States.
By contrast, the study by Lisa Littman sought respondents from a political and ideological variety of sources.
In a recent retrospective case-note review3, performed as a service evaluation over twelve months, 6.9% of participants met the case definition of detransitioning, yet 21.7% disengaged from the study.
In general, detransitioners remain an underserved population in healthcare, with far more research required to understand their needs4.
- Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Arch Sex Behav. [Link] ↩︎
- Turban, J.L., Loo, S.S., Almazan, A.N., & Keuroghlian, A.S. (2021). Factors Leading to “Detransition” Among Transgender and Gender Diverse People in the United States: A Mixed-Methods Analysis. LGBT health 8(4): 273-280. [Link] ↩︎
- Hall, R., Mitchell, L., & Sachdeva, J. (2021). Access to care and frequency of detransition among a cohort discharged by a UK national adult gender identity clinic: Retrospective case-note review. BJPsych Open 7(6): E184. [Link] ↩︎
- Expósito-Campos, P. (2021). A Typology of Gender Detransition and Its Implications for Healthcare Providers. Journal of Sex & Marital Therapy 47 (3): 270-280. [Link] ↩︎
-
Transmen are four or five times more likely than females in general to suffer a heart attack
A 2019 study1 found that post-operative female-to-male transgender people were 4.9 times as likely to suffer a myocardial infarction (heart attack) than women in general.
Another study2 also found a somewhat smaller yet still large discrepancy, concluding that transmen were 3.69 more likely to suffer a heart attack than women in general.
- Alzahrani, T. Nguyen, T., Ryan, A., Dwairy, A. McCaffrey, J., Yunus, R., Forgione, J., Krepp, J., Nagy, C., Mazhari, R. & Reiner, J. (2019). Cardiovascular Disease Risk Factors and Myocardial Infarction in the Transgender Population. Circulation: Cardiovascular Quality and Outcomes 12 (4). [Link] ↩︎
- Nota, N.M., Wiepjes, C.M., de Blok, C.J.M., Gooren, L.J.G., Kreukels, B.P.D. & den Heijer, M. (2019). Occurrence of Acute Cardiovascular Events in Transgender Individuals Receiving Hormone Therapy: Results From a Large Cohort Study. Circulation 139: 1461-1462. [Link] ↩︎
-
Young transgender people are at elevated risk of contracting HIV and other STDs
Transgender adolescents and young adults, particularly trans females, are at a disproportionately high risk of contracting human immunodeficiency virus1 and other sexually transmitted diseases2.
- Poteat, T., Scheim, A., Xavier, J., Reisner, S. & Baral, S. (2016). Global Epidemiology of HIV Infection and Related Syndemics Affecting Transgender People. Journal of Acquired Immune Deficiency Syndromes 72 (Suppl 3). [Link] ↩︎
- Reisner, S.L., Vetters, R., Leclerc, M., Zaslow, S., Wolfrum, S., Shumer, D. & Mimiaga, M.J. (2015). Mental Health of Transgender Youth in Care at an Adolescent Urban Community Health Center: A Matched Retrospective Cohort Study. Journal of Adolescent Health 56 (3): 274-279. [Link] ↩︎
-
There is evidence that it is harder to sustain meaningful sexual relationships after medical transition
A study1 on informed consent found that male-to-female transitioners who are attracted to men may discover that men who are sexually interested in them are specifically interested in their trans status, and have no interest in serious long-term relationships.
The same study noted that male-to-female transitioners who are attracted to women may find that lesbians are unwilling to engage in a sexual relationship with a male.
Because most female-to-male transitioners do not undergo phalloplasty, their ability to attract desirable sexual partners, and sustain relationships with them, could be compromised.
Only a single case2 of a female-to-male transitioner treated with puberty blockers followed by cross-sex hormones and surgeries has feen followed long-term.
The individual, who was in his thirties during the follow up, reported an inability to have a satisfying sexual life due to “shame about his genital appearance and his feelings of inadequacy in sexual matters”. The researchers concluded, that despite the gender reassignment, “in the area of intimate relationships, it may remain difficult to find a suitable partner”.
- Levine, S. (2018). Informed Consent for Transgendered Patients. Journal Of Sex & Marital Therapy, 45(3), 218-229. [Link] ↩︎
- Cohen-Kettenis, P., Schagen, S., Steensma, T., de Vries, A., & Delemarre-van de Waal, H. (2011). Puberty Suppression in a Gender-Dysphoric Adolescent: A 22-Year Follow-Up. Archives Of Sexual Behavior 40 (4): 843-847. [Link] ↩︎
-
Medical transition reduces dating pool size and likelihood of marriage
Individuals undergoing biomedical interventions to address their gender dysphoria are at risk for having a greatly diminished pool of individuals who are willing to sustain an intimate physical and loving relationship1.
This is evidenced in the much lower marriage rates of transgender adults2.
- Levine, S. (2018). Informed Consent for Transgendered Patients. Journal Of Sex & Marital Therapy, 45(3), 218-229. [Link] ↩︎
- Yarbrough, E. (2018). Transgender mental health. Washington, DC: American Psychiatric Association Publishing. [Link] ↩︎
-
There is evidence that up to a quarter of transgender genital surgeries result in incontinence
A systematic literature review1 found that 21% of male-to-female patients and 25% of female-to-male patients suffered from incontinence as a result of transgender genital surgery.
One recent study2 estimates the number of post-operative transsexuals suffering stress incontinence to be 23%. This study was not a literature review, and almost all of the participants were male-to-female.
- Nassiri, N., Maas, M., Basin, M., Cacciamani, G.E. & Doumanian, L.R. (2020). Urethral complications after gender reassignment surgery: a systematic review. Int J Impot Res. [Link] ↩︎
- Kuhn, A., Santi, A. & Birkhäuser, M. (2011). Vaginal prolapse, pelvic floor function, and related symptoms 16 years after sex reassignment surgery in transsexuals. Fertil Steril. 95: 2379-82. [Link] ↩︎
-
Around 1 in 5 vaginoplasty surgeries lead to corrective surgery
A systematic review1 of neo-vagina surgeries found a re-operation rate of 21.7% for non-esthetic reasons.
A Brazilian paper2 found a somewhat lower, but similar, reoperation rate of 16.8%.
- Dreher, P.C., Edwards, D., Hager, S., Dennis, M., Belkoff, A., Mora, J., Tarry, S. & Rumer, K.L. (2018). Complications of the neovagina in male-to-female transgender surgery: A systematic review and meta-analysis with discussion of management. Clin Anat. 31 (2):191-199. [Link] ↩︎
- Moisés da Silva, G.V., Lobato, M.I.R., Silva, D.C., Schwarz, K., Fontanari, A.M.V., Costa, A.B., Tavares, P.M., Gorgen, A.R.H., Cabral, R.D. & Rosito, T.E. (2021). Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Frontiers in Surgery 8. [Link] ↩︎
-
Vaginoplasty can result in fistula, stenosis, necrosis, prolapse and even death
Male-to-female genital surgery (vaginoplasty) is associated with significant long-term complications: there is a 2% risk of fistula, 14% risk of stenosis (abnormal narrowing), 1% risk of necrosis (tissue death) and 4% risk of prolapse1.
One systematic review2 found an overall complication rate of 32.5%.
A Dutch study3 of 55 (out of an original 70) adolescents treated with puberty blockers, cross sex hormones, and genital surgery, showed that among 22 male-to-female patients who underwent vaginoplasty, one adolescent died as a result of necrotizing fasciitis after the surgery.
- Manrique, O., Adabi, K., Martinez-Jorge, J., Ciudad, P., Nicoli, F. and Kiranantawat, K. (2018). Complications and Patient-Reported Outcomes in Male-to-Female Vaginoplasty—Where We Are Today. Annals of Plastic Surgery 80 (6): 684-691. [Link] ↩︎
- Dreher, P.C., Edwards, D., Hager, S., Dennis, M., Belkoff, A., Mora, J., Tarry, S. & Rumer, K.L. (2018). Complications of the neovagina in male-to-female transgender surgery: A systematic review and meta-analysis with discussion of management. Clin Anat. 31 (2):191-199. [Link] ↩︎
- de Vries, A., McGuire, T., Steensma, E., Wagenaar, T., Doreleijers, P. & Cohen-Kettenis, P. (2014). Young adult psychological outcome after puberty suppression and gender reassignment. [Link] ↩︎
-
Feminizing hormones reduce sexual function in males
Feminizing hormonal treatments lead to a lessening drive, erectile dysfunction, and shrinking of testes and penis1, significantly compromising sexual function.
A Belgian doctoral thesis study2 found that 69.7% of transwomen reported a decrease in sexual desire — while the opposite effect is found in transmen.
- Levine, S. (2018). Informed Consent for Transgendered Patients. Journal Of Sex & Marital Therapy, 45(3), 218-229. [Link] ↩︎
- Elaut, E. (2014). Biopsychosocial factors in the sexual desire of contraception‐using couples and trans persons. Doctoral thesis, University of Ghent. [Link] ↩︎
-
Genital surgeries tend to reduce the capacity for orgasm in males, and may do so in females
One study showed that around 30% of male-to-female genital surgeries result in the inability to orgasm1.
Figures on female-to-male transitioners are less clear. However, a clinical follow-up study2 of 38 transmen – 29 of whom had received phalloplasty, and 9 metoidioplasty – found that reported loss of orgasmic capacity was more marginally common than reported gain of orgasmic capacity.
The negative intrapsychic and interpersonal consequences of anorgasmia (the inability to climax) is well-documented, and applies equally to transgender individuals3.
- Manrique, O., Adabi, K., Martinez-Jorge, J., Ciudad, P., Nicoli, F. and Kiranantawat, K. (2018). Complications and Patient-Reported Outcomes in Male-to-Female Vaginoplasty—Where We Are Today. Annals of Plastic Surgery 80 (6): 684-691. [Link] ↩︎
- van de Grift, T., Pigot, G., Kreukels, B., Bouman, M., & Mullender, M. (2019). Transmen’s Experienced Sexuality and Genital Gender-Affirming Surgery: Findings From a Clinical Follow-Up Study. Journal Of Sex & Marital Therapy 45 (3): 201-205. [Link] ↩︎
- Levine, S. (2018). Informed Consent for Transgendered Patients. Journal Of Sex & Marital Therapy, 45(3), 218-229. [Link] ↩︎
-
In one study, 11% of transmen who took testosterone developed a condition called erythrocytosis, which impacts red blood cells and slows the blood flow
A study1 of 776 transmen who took testosterone demonstrated that 11% of them developed erythrocytosis, a condition which slows the blood flow, and can lead to headaches, confusion, high blood pressure, nosebleeds, blurred vision, itching and fatigue.
- Madsen, M.C., van Dijk, D. Wiepjes, C.M., Conemans, E.B., Thijs, A. & den Heijer, M. (2021). Erythrocytosis in a Large Cohort of Trans Men Using Testosterone: A Long-Term Follow-Up Study on Prevalence, Determinants, and Exposure Years. The Journal of Clinical Endocrinology & Metabolism 106 (6): 1710–1717. [Link] ↩︎
-
Long-term testosterone use in natal females can cause vaginal atrophy, which makes sex painful
A study1 of 16 female-to-male transgender individuals concluded that long-term testosterone administration leads to vaginal atrophy (Baldassarre et al., 2013). The study noted that:
Vaginal samples from FtM showed a loss of normal architecture of the epithelium, intermediate and superficial layers were completely lost, and glycogen content was depleted.
Vaginal atrophy, characterized by thinning of vaginal walls and poor lubrication of vaginal tissues, leads to tearing, micro abrasions, bleeding, and painful intercourse.
- Baldassarre, M., Giannone, F., Foschini, M., Battaglia, C., Busacchi, P., Venturoli, S., & Meriggiola, M. (2013). Effects of long-term high dose testosterone administration on vaginal epithelium structure and estrogen receptor-α and -β expression of young women. International Journal Of Impotence Research, 25 (5): 172-177. [Link] ↩︎
-
Medical transition puts both males and females at risk of infertility
A wide-ranging study1 found that gender-related drug regimens place patients at risk of infertility:
Suppression of puberty with gonadotropin-releasing hormone agonist analogs (GnRHa) in the pediatric transgender patient can pause the maturation of germ cells, and thus, affect fertility potential. Testosterone therapy in transgender men can suppress ovulation and alter ovarian histology, while estrogen therapy in transgender women can lead to impaired spermatogenesis and testicular atrophy. The effect of hormone therapy on fertility is potentially reversible, but the extent is unclear.
On surgeries, the study noted that cross-sex surgery that includes hysterectomy and oophorectomy in transmen or orchiectomy in transwomen results in permanent sterility.
- Cheng, P.J., Pastuszak, A.W., Myers, J.B., Goodwin, I.A. & Hotaling, J.M. (2019). Fertility concerns of the transgender patient. Transl Androl Urol. 8 (3): 209-218. [Link] ↩︎
-
One study found that puberty blockers did not alleviate negative thoughts in children with gender dysphoria
A British study1 found that puberty blockers used to treat children aged 12 to 15 who have severe and persistent gender dysphoria had no significant effect on their psychological function, thoughts of self-harm, or body image.
However, as expected, the children experienced reduced growth in height and bone strength by the time they finished their treatment at age 16.
- Carmichael, P., Butler, G., Masic, U., Cole, T. J., De Stavola, B. L., Davidson, S., Skageberg, E. M., Khadr, S., & Viner, R. M. (2021). Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLOS ONE 16 (2). [Link] ↩︎
-
Puberty blockers and cross-sex hormones negatively impact bone health in a significant number of cases
There is little long-term evidence on bone mass density in relation to puberty blockers. However, in a significant minority of cases of long-term puberty suppression related to gender identity, bone mass density scores qualify as “low for age”1. Low bone mass density increases risk of osteoporosis and fractures.
Adolescents who enter puberty at an older age have persistently lower bone mass density than their peers2: in one case study3, an adolescent had a bone mass density -2 standard deviations below the mean after three years of blocking puberty.
It has also been noted4 that:
In early-pubertal transgender youth, BMD [bone mass density] was lower than reference standards for sex designated at birth. This lower BMD may be explained, in part, by suboptimal calcium intake and decreased physical activity–potential targets for intervention.
Bone metabolism is also decreased as a result of taking cross-sex hormones, for both males and (in later life) females5.
- Biggs, M. (2021). Revisiting the effect of GnRH analogue treatment on bone mineral density in young adolescents with gender dysphoria. Journal of Pediatric Endocrinology and Metabolism 34 (7): 937-939. [Link] ↩︎
- Elhakeem, A., Frysz, M., Tilling, K., Tobias, J.H. & Lawlor, D.A. (2019). Association Between Age at Puberty and Bone Accrual From 10 to 25 Years of Age. JAMA Netw Open; 2(8). [Link] ↩︎
- Pang, K.C., Notini, L., McDougall, R., Gillam, L., Savulescu, J., Wilkinson, D., Clark, B.A., Olson-Kennedy, J., Telfer, M.M. & Lantos, J.D. (2020). Long-term Puberty Suppression for a Nonbinary Teenager. Pediatrics 145 (2). [Link] ↩︎
- Lee, J. Y., Finlayson, C., Olson-Kennedy, J., Garofalo, R., Chan, Y. M., Glidden, D. V., & Rosenthal, S. M. (2020). Low Bone Mineral Density in Early Pubertal Transgender/Gender Diverse Youth: Findings From the Trans Youth Care Study. Journal of the Endocrine Society 4 (9). [Link] ↩︎
- Vlot, M.C., Wiepjes, C.M., de Jongh, R.T., T’Sjoen, G., Heijboer, A.C. & den Heijer, M. (2019). Gender-Affirming Hormone Treatment Decreases Bone Turnover in Transwomen and Older Transmen. J Bone Miner Res, 34: 1862-1872. [Link] ↩︎
-
The chances of developing osteoporosis and cardiovascular problems increase with feminizing hormones
A 2012 paper1 found that a quarter of the male-to-female transsexuals it studied had osteoporosis at the lumbar spine and radius.
In the same study, 6% of male-to-female transsexuals experienced a thromboembolic event (a blood clot causing obstruction), and another 6% experienced other cardiovascular problems. These effects were observed after only 11.3 years of hormone treatment on average.
A further study2 found that long-term bone mineral density decreases in transwomen who take cross-sex hormones in the long term.
- Wierckx, K., Mueller, S., Weyers, S., Van Caenegem, E., Roef, G., Heylens, G. & T’Sjoen, G. (2012). Long-Term Evaluation of Cross-Sex Hormone Treatment in Transsexual Persons. The Journal of Sexual Medicine 9 (10): 2641-2651. [Link] ↩︎
- Delgado-Ruiz, R., Swanson, P., & Romanos, G. (2019). Systematic Review of the Long-Term Effects of Transgender Hormone Therapy on Bone Markers and Bone Mineral Density and Their Potential Effects in Implant Therapy. Journal of clinical medicine 8 (6): 784. [Link] ↩︎
-
Female-to-male genital reconstruction surgery has a high negative outcome rate, including urethral compromise and worsened mental health
The results of a 2021 international survey1 of 129 female-to-male patients who underwent genital reconstruction surgery support anecdotal reports that complication rates following genital reconstruction are higher than are commonly reported in the surgical literature.
Complication rates, including urethral compromise, and worsened mental health outcomes remain high for gender affirming penile reconstruction. In total, the 129 patients reported 281 complications requiring 142 revisions.
Another paper2 found a 70% complication rate in one type of female-to-male genital reconstruction surgery.
Even with the “radial forearm free flap” method of creating a synthetic penis — “considered by many as the gold standard for phalloplasty”3 — there are high rates of complications, with up to 64% urethroplasty related complications4.
- Robinson, I.S., Blasdel, G., Cohen, O., Zhao, L.C. & Bluebond-Langner, R. (2021). Surgical Outcomes Following Gender Affirming Penile Reconstruction: Patient-Reported Outcomes From a Multi-Center, International Survey of 129 Transmasculine Patients. J Sex Med 18 (4): 800-811. [Link] ↩︎
- Bettocchi, C., Ralph, D.J. & Pryor, J.P. (2005). Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95:120–4. [Link] ↩︎
- Rashid, M. & Tamimy, M. S. (2013). Phalloplasty: The dream and the reality. Indian J Plast Surg 46 (2): 283-293. [Link] ↩︎
- Fang, R.H., Lin, J.T. & Ma S. (1994). Phalloplasty for female transsexuals with sensate free forearm flap. Microsurgery 15: 349–52. [Link] ↩︎
-
There is little evidence that medical transition decreases suicidality
When it comes to gender dysphoric children, there is little evidence that medical transition decreases suicide rates. There is little evidence to assert that puberty blockers are necessary to prevent suicide1.
After sex reassignment surgery, one study showed that adult transsexual clients were 4.9 times more likely to have made a suicide attempt and 19.1 times more likely to have died from suicide, after adjusting for prior psychiatric comorbidity2. Similarly, an Australian paper3 notes that many patients have poor outcomes, which puts them at risk of suicide.
A prominent study4 claiming that medical transition alleviated suicidality had to be corrected5, to clarify that it proved “no advantage of surgery” in this regard.
A long-term Swedish study6 finds that post-operative transgender people have “considerably higher risks” for suicidal behavior.
Similarly, a study in the European Journal of Endocrinology7 demonstrates that suicide rates among transgender male-to-females were 51% higher than the general population.
- Biggs, M. (2020). Puberty Blockers and Suicidality in Adolescents Suffering from Gender Dysphoria. Archives of Sexual Behavior (49): 2227–2229. [Link] ↩︎
- Zucker, K.J., Lawrence, A.A., Kreukels, B.P. (2016). Gender Dysphoria in Adults. Annu Rev Clin Psychol. 12: 217-47. [Link] ↩︎
- D’Angelo, R. (2018). Psychiatry’s ethical involvement in gender-affirming care. Australasian Psychiatry 26 (5): 460-463. [Link] ↩︎
- Bränström, R. & Pachankis, J. E. (2019). Reduction in Mental Health Treatment Utilization Among Transgender Individuals After Gender-Affirming Surgeries: A Total Population Study. American Journal of Psychiatry 177 (8): 727-734. [Link] ↩︎
- American Journal of Psychiatry (2020). Correction to Bränström and Pachankis. Published online: 1 August 2020. [Link] ↩︎
- Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L. V., Långström, N., & Landén, M. (2011). ‘Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study in Sweden’. PLoS ONE, 6(2). [Link] ↩︎
- Asscheman, H., Giltay, E. J., Megens, J. A. J., de Ronde, W., van Trotsenburg, M. A. A. & Gooren, L. J. G. (2011). A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. European Journal of Endocrinology 164 (4). [Link] ↩︎
-
Suicide rarely has one cause: it is difficult for statistical studies on suicide to extricate gender dysphoria from other factors
A Swedish study1 points out that it is “difficult to distinguish one [gender dysphoria] from the other [mental health conditions] with regard to suicide risk.”
A 2019 study2 finds that “adolescents referred for gender dysphoria show higher rates of suicidality when compared to non-referred adolescents, but are much more similar to referred adolescents (presumably, the vast majority were cisgender) in general.”
- Swedish National Board of Health and Welfare (2020). Utvecklingen av diagnosen könsdysfori: Förekomst, samtidiga psykiatriska diagnoser och dödlighet i suicid. Socialstyrelsen. [Link] ↩︎
- Zucker, K. J. (2019). Adolescents with Gender Dysphoria: Reflections on Some Contemporary Clinical and Research Issues. Archives of Sexual Behavior 48 (5). [Link] ↩︎
-
People with psychiatric conditions – and sometimes neurodiverse conditions – are much more likely to die by suicide than gender dysphoric people
A Swedish study1 found that suicide rates for personality disorder, schizophrenia, substance addiction, bipolar and (among males) depression and autism were all higher than suicide rates for gender dysphoric people:

These high suicide rates for schizophrenia are confirmed by another study2 which puts the lifetime risk of suicide death for schizophrenics at 5.6%. This study also finds “the absolute risk of suicide in different psychiatric disorders to vary from 2% to 8%, higher for men than for women and highest for men and women with bipolar disorder, unipolar affective disorder, schizophrenia, and schizophrenialike disorder.”
- Swedish National Board of Health and Welfare (2020). Utvecklingen av diagnosen könsdysfori: Förekomst, samtidiga psykiatriska diagnoser och dödlighet i suicid. Socialstyrelsen. [Link] ↩︎
- Nordentoft, M., Madsen, T. & Fedyszyn, I. (2015). Suicidal behavior and mortality in first-episode psychosis. J Nerv Ment Dis. 203 (5): 387-92. [Link] ↩︎
-
There is no high quality evidence to suggest that the overall attempted suicide rate of transgender youth is 41%
The frequently repeated claim that 41% of 6,450 transgender respondents said they had attempted suicide at some point in their lives1 is taken from the National Transgender Discrimination Survey2.
However, a 2021 paper3 notes that the participants were recruited through transgender advocacy organizations and subjects were asked to “pledge” to promote the survey among friends and family. This recruiting method yielded a large but highly skewed sample. By targeting transgender advocacy groups, the survey underrepresented the experiences of transgender individuals who are not politically engaged. Also, a very high number of the survey participants (nearly 40%) had not transitioned medically or socially at the time of the survey, and a significant number reported no intention to transition in the future.
A 2016 article4 analyzes the power of this 41% statistic, investigating how it has affected conversations about the injustices transgender people face and the importance of family and societal acceptance.
- Turban, J. L., Beckwith, N., Reisner, S. L., & Keuroghlian, A. S. (2020). Association between recalled exposure to gender identity conversion efforts and psychological distress and suicide attempts among transgender adults. JAMA Psychiatry 77 (1): 68-76. [Link] ↩︎
- Grant, J. M., Mottet, L. A., Tanis, J., Harrison, J., Herman, J. L., & Keisling, M. (2011). Injustice at every turn: A report of the national transgender discrimination survey. National Gay and Lesbian Task Force; National Center for Transgender Equality. [Link] ↩︎
- D’Angelo, R., Syrulnik, E., Ayad, S., Marchiano, L., Kenny, D.T. & Clarke, P. (2021). One Size Does Not Fit All: In Support of Psychotherapy for Gender Dysphoria. Arch Sex Behav 50: 7-16. [Link] ↩︎
- Tanis, J. (2016). The power of 41%: A glimpse into the life of a statistic. Am J Orthopsychiatry, 86 (4): 373-7. [Link] ↩︎
-
One long-ranging study estimated a suicide rate for gender dysphoric people of 0.6%
Every suicide is a tragedy, and one suicide is a suicide too many. With such a serious issue, accuracy is critical.
A Swedish government-commissioned study1 found that 39 of 6334 gender dysphoric individuals — 0.6% — died by suicide.
The UK’s largest gender clinic, the Gender Identity Development Service, states that2
Suicide is extremely rare.
Similarly, the Chair of the Child and Adolescent Committee for the World Professional Association for Transgender Health (WPATH), Dr Laura Edwards-Leeper, remarks3:
As far as I know there are no studies that say that if we don’t start these kids immediately on hormones when they say they want them that they are going to commit suicide. So that is misguided…in terms of needing to intervene medically to prevent suicide and doing it quickly, I know of no studies that have shown that.
This reinforces the point that talking about suicide is not the same as dying by suicide. While there is evidence4 that suicidal ideation is higher among gender-dysphoric youth than in the general population, an increase in suicidal ideation rates is not proof of an equal increase in suicide rates themselves.
However, the way suicidality is reported can affect numbers of suicides. A significant body of academic research from across the world, known as the Werther Effect, has found links between certain types of reporting of suicides and increased suicide rates5.
- Swedish National Board of Health and Welfare (2020). Utvecklingen av diagnosen könsdysfori: Förekomst, samtidiga psykiatriska diagnoser och dödlighet i suicid. Socialstyrelsen. [Link] ↩︎
- Gender Identity Development Service (2021). Evidence base. [Link] ↩︎
- Daum, Meghan (2021). “We Feel Like We’re In The Wild West:” Parents of Gender-Questioning Kids Ask Their Own Questions. The Unspeakable Podcast, October 4, 2021. [Link] ↩︎
- Aitken, M., Vanderlaan, D., Wasserman, L., Stojanovski, S. & Zucker, K. (2016). Self-Harm and Suicidality in Children Referred for Gender Dysphoria. Journal of the American Academy of Child & Adolescent Psychiatry 55. [Link] ↩︎
- Acosta, F. J., Rodríguez, C. J., Cejas, M. R., Ramallo-Fariña, Y. & Fernandez-Garcimartin, H. (2020) Suicide Coverage in the Digital Press Media: Adherence to World Health Organization Guidelines and Effectiveness of Different Interventions Aimed at Media Professionals. Health Communication 35 (13). [Link] ↩︎
-
There is evidence that all-cause mortality is higher among trans people than among the general population
A Swedish study1 found that sex-reassigned transsexual persons – both male and female – had approximately a three times higher risk of all-cause mortality than non-transsexuals. Elevated causes of mortality included cancer, cardiovascular disease, and violent crime:

This finding was backed up by a Dutch study2, which stated:
This observational study showed an increased mortality risk in transgender people using hormone treatment, regardless of treatment type. This increased mortality risk did not decrease over time.
- Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L. V., Långström, N., & Landén, M. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study in Sweden. PLoS ONE, 6(2). [Link] ↩︎
- de Blok, C.J.M., Wiepjes, C.M., van Velzen, D.M., Staphorsius, A.S., Nota, N.M., Gooren, L.J.G., Kreukels, B.P.C. & den Heijer, M. (2021). Mortality trends over five decades in adult transgender people receiving hormone treatment: a report from the Amsterdam cohort of gender dysphoria. The Lancet Diabetes & Endocrinology 9. [Link] ↩︎
-
Young people who desist from a trans identity are disproportionately likely to grow up to be non-heterosexual
A Dutch paper1 notes that, for gender dysphoric children, the more likely psychosexual outcome in adulthood is a homosexual sexual orientation without gender dysphoria.
Evidence2 suggests that many boys whose childhood gender dysphoria recedes with puberty will grow up to be bisexual or homosexual. Another study of males3 indicates that bisexual/homosexual orientation is far greater than base rates in the general male population, with 63.6% of boys with gender identity disorder being same-sex attracted.
This suggests that a non-heterosexual orientation is particularly likely among gender dysphoric boys.
- Wallien, M.S. & Cohen-Kettenis P.T. (2008) Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry 47 (12): 1413-23. [Link] ↩︎
- Kaltiala-Heino, R., Bergman, H., Työläjärvi, M., & Frisén, L. (2018). Gender dysphoria in adolescence: current perspectives. Adolescent health, medicine and therapeutics 9, 31–41. [Link] ↩︎
- Singh, D. (2012). A follow-up study of boys with gender identity disorder. Doctoral thesis, University of Toronto. [Link] ↩︎
-
Gender-related distress will alleviate for around 80% of pre-teen children once they become teenagers
Evidence from 10 available prospective follow-up studies1 from childhood to adolescence indicates that childhood gender dysphoria will recede with puberty in ~80% of cases. A Dutch paper2 notes that follow-up studies show the persistence rate of gender identity disorder to be about 15.8%, or 39 out of the 246 children who were reported on in the literature.
In one study3 of 54 children referred to a clinic in childhood because of gender dysphoria and then later investigated by a follow-up study, only 21 (39%) still had gender dysphoria.
A different study4 of Canadian boys with gender identity disorder showed that 87.8% desisted, with only 12.2% — fewer than 1 in 8 — persisting in their transgender identity.
An ~80% desistance is not universally found5. Thorough investigations of the claims and counter-claims appear in two 2018 studies67.
- Kaltiala-Heino, R., Bergman, H., Työläjärvi, M., & Frisén, L. (2018). Gender dysphoria in adolescence: current perspectives. Adolescent health, medicine and therapeutics 9, 31–41. [Link] ↩︎
- Steensma, T.D. & Cohen-Kettenis, P.T. (2011). Gender Transitioning before Puberty? Archives of Sexual Behavior 40 (4): 649-50. [Link] ↩︎
- Wallien, M.S. & Cohen-Kettenis P.T. (2008) Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry 47 (12): 1413-23. [Link] ↩︎
- Singh, D., Bradley, S.J. & Zucker, K.J. (2021). A Follow-Up Study of Boys With Gender Identity Disorder. Frontiers in Psychology 12. [Link] ↩︎
- Temple Newhook, J., Pyne, J., Winters, K., Feder, S., Holmes, C., Tosh, J., Sinnott, M., Jamieson, A., & Picket, S. (2018). A critical commentary on follow-up studies and “desistance” theories about transgender and gender non-conforming children. International Journal of Transgenderism 19 (2). [Link] ↩︎
- Steensma, T.D. & Cohen-Kettenis, P.T. (2018). A critical commentary on “A critical commentary on follow-up studies and “desistence” theories about transgender and gender non-conforming children”. International Journal of Transgenderism. [Link] ↩︎
- Zucker, K. J. (2018). The myth of persistence. International Journal of Transgenderism 19 (2): 231-45. [Link] ↩︎
-
Studies on gender dysphoric young people often suffer from high rates of loss to follow-up – which could skew transition satisfaction rates
In one study1 of 77 pre-teen participants, 30% were lost to follow up by their teenage years: either they did not respond to the recruiting letter, or were not traceable. In another study2, as many as 75% of participants were lost to follow up.
An excellent précis of this problem can be found in a 2018 paper3, which gives further detail:
Smith et al. report that sex reassignment is effective, based on a study of 162 adults who had undergone SRS. They were able to obtain follow-up data from only 126 (78%) of subjects because a significant number were “untraceable” or had moved abroad.
De Cuypere et al. report that sex reassignment surgery is an effective treatment for transsexuals. Of 107 patients who had undergone SRS between 1986 and 2001, 30 (28%) could not be contacted and 15 (14%) refused to participate.
Johannson et al. reported good outcomes for SRS. Of 60 patients who had undergone SRS, 42 (70%) agreed to participate in the follow up research. Of the non-participants, 1 had died of complications of SRS, 8 could not be contacted and 9 refused to participate.
Salvador et al. reported that SRS has a positive effect on psychosocial functioning. Only 55 of the 69 patients (80%) could be contacted as 17 were lost to follow-up
Van de Grift et al. reported 94–96% of patients are satisfied with SRS and have good quality of life. A total of 546 patients with Gender Dysphoria who had applied for SRS at clinics in Amsterdam, Hamburg and Ghent were contacted to complete an online survey. Only 201 (37%) responded and completed the survey.
A good example of how this phenomenon can affect satisfaction and regret statistics comes from a 2018 paper4, which is often cited as proof of low regret rates. The loss to follow up rate in this paper is 36%. The authors also state:
In addition, in our population the average time to regret was 130 months, so it might be too early to examine regret rates in people who started with HT [hormonal treatment] in the past 10 years.
- Wallien, M.S. & Cohen-Kettenis P.T. (2008) Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry 47 (12): 1413-23. [Link] ↩︎
- Rauchfleisch, U., Barth, D. & Battegay, R. (1998). Resultate einer Langzeitkatamnese von Transsexuellen. Der Nervenzart 69: 799-805. [Link] ↩︎
- D’Angelo, R. (2018). Psychiatry’s ethical involvement in gender-affirming care. Australasian Psychiatry 26 (5): 460-463. [Link] ↩︎
- Wiepjes, C.M., Nota, N.M., de Blok, C.J.M., Klaver, M., de Vries, A.L.C., Wensing-Kruger, S.A., de Jongh, R.T., Bouman, M.B., Steensma, T.D., Cohen-Kettenis, P., Gooren, L.J.G., Kreukels, B.P.C. & den Heijer, M. (2018). The Amsterdam Cohort of Gender Dysphoria Study (1972-2015): Trends in Prevalence, Treatment, and Regrets. Journal of Sexual Medicine 15 (4). [Link] ↩︎
-
There is limited evidence that medical transition leads to positive outcomes
A number of different studies have noted the paucity of good quality evidence for transition.
An Australian paper1 states that most available evidence indicating positive outcomes for gender reassignment is of poor quality.
A German study2 “found insufficient evidence to determine the efficacy or safety of hormonal treatment approaches for transgender women in transition”, adding that “[t]his lack of studies shows a gap between current clinical practice and clinical research.”
A British review3 conducted by the National Institute for Health and Care Excellence (NICE) graded certainty of evidence for puberty blocker use as “very low” in every category, including impact on gender dysphoria, mental health, body image, global functioning, psychosocial functioning, cognitive functioning, bone density and adverse effects.
A chapter4 in an edited volume details the low evidence base for treatment pathways employed at the UK’s Gender Identity Development Service, demonstrating how negative evidence was “ignored or suppressed”.
Finally, a systematic review5 commissioned by the World Professional Association for Transgender Health (WPATH) to “systematically review the effect of gender-affirming hormone therapy on psychological outcomes among transgender people” noted that, in some areas, there was low quality or insufficient evidence.
- D’Angelo, R. (2018). Psychiatry’s ethical involvement in gender-affirming care. Australasian Psychiatry 26 (5): 460-463. [Link] ↩︎
- Haupt, C., Henke, M., Kutschmar, A., Hauser, B., Baldinger, S., Saenz, S.R. & Schreiber, G. (2020). Antiandrogen or estradiol treatment or both during hormone therapy in transitioning transgender women. Cochrane Database of Systematic Reviews 11. [Link] ↩︎
- National Institute for Health and Care Excellence (2021). Evidence review: Gonadotrophin releasing hormone analogues for children and adolescents with gender dysphoria. National Institute for Health and Care Excellence (NICE); NHS England; NHS Improvement. [Link] ↩︎
- Biggs, M. (2019). The Tavistock’s Experiment with Puberty Blockers. In: Moore, M. & Brunskell-Evans, H. (eds.). Inventing Transgender Children and Young People. Cambridge Scholars Publishing. [Link] ↩︎
- Baker, K.E., Wilson, L.M., Sharma, R., Dukhanin, V., McArthur, K. & Robinson, K.A. (2021) Hormone Therapy, Mental Health, and Quality of Life Among Transgender People: A Systematic Review. Journal of the Endocrine Society 5 (4). [Link] ↩︎
-
There is no evidence that English historically used ‘they’ to refer to a named and known individual
For centuries, the English language has used ‘they’ as an epicene pronoun (i.e. to mean ‘he or she’). This epicene use is shared by authors from Shakespeare to Austen and Shelley1.
However, epicene use of ‘they’ rules out knowledge of the identity — and thus the sex — of the person in question. In other words, this historical use of singular ‘they’ is restricted to contexts where ‘they’ refers to an unknown party, rather than to a particular named and known individual.
There is no literature on the use of definite singular ‘they’ (i.e. to refer to a named and known person) before 20172.
Furthermore, the research undertaken in 20173 indicates that many English speakers who naturally use epicene ‘they’ find it difficult to parse uses of ‘they’ to refer to a named and known singular individual.
- Grubber, B. (2017). Singular They: The Best Epicene Pronoun. Student Research Conference Select Presentations: Paper 45. [Link] ↩︎
- Konnelly, L. & Cowper, E. (2020). Gender diversity and morphosyntax: An account of singular they. Glossa: a journal of general linguistics 5 (1): 1–19. [Link] ↩︎
- Bjorkman, B.M. (2017). Singular they and the syntactic representation of gender in English. Glossa: a journal of general linguistics 2 (1): 1-13. [Link] ↩︎
-
Transgender-identified youth are disproportionately likely to suffer from eating disorders
In a review1 of 20 publications, significantly higher rates of eating disorder symptoms were documented in transgender youth (aged between 8 and 25).
Another study2 corroborated this connection, noting that data, while scarce, suggest “an overrepresentation of eating pathology among adolescents with GD [gender dysphoria] or transgender identity.”
- Coelho, J., Suen, J., Clark, B., Marshall, S., Geller, J. & Lam, P.-Y. (2019). Eating Disorder Diagnoses and Symptom Presentation in Transgender Youth: a Scoping Review. Current Psychiatry Reports 21. [Link] ↩︎
- Kaltiala-Heino, R., Bergman, H., Työläjärvi, M., & Frisén, L. (2018). Gender dysphoria in adolescence: current perspectives. Adolescent health, medicine and therapeutics 9, 31–41. [Link] ↩︎
-
Transgender-identified youth are prone to elevated rates of depression and/or anxiety
A study1 which compared the medical records of 1333 trans-identified children and adolescents between the ages of 3 and 17 years old with a similar cohort of non-trans-identified children and adolescents showed that 49% of males and 62% of females had depressive disorders.
An Australian study2, with a smaller sample of gender dysphoric children and adolescents, found depression and anxiety rates of 62.0% and 63.3% respectively.
The majority of parent respondents in Littman’s 2018 study3 – 69.4% – answered that their child had social anxiety during adolescence; 44.3% said that their child had difficulty interacting with their peers, and 43.1% that their child had a history of being isolated (not associating with their peers outside of school activities).
Similar conclusions have been found4 for adults with gender dysphoria, who suffer from elevated rates of mood disorders (48.9% among natal males, 36.1% among natal females) and anxiety (38.8% among natal males, 33.3% among natal females). A further paper5 found somewhat lower figures, giving a prevalence of 42.1% for mood disorders and 26.8% for anxiety disorders.
- Becerra-Culqui, T.A. Liu, Y., Nash, R., Cromwell, L., Flanders, W.D., Getahun, D. Giammattei, S.V., Hunkeler, E.M., Lash, T.L., Millman, A., Quinn, V.P., Robinson, B., Roblin, D., Sandberg, D.E., Silverberg, M.J., Tangpricha, V. & Goodman, M. (2018). ‘Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics 141(5). [Link] ↩︎
- Kozlowska, K., McClure, G., Chudleigh, C., Maguire, A.M., Gessler, D., Scher, S. & Ambler, G.R. (2021). ‘Australian children and adolescents with gender dysphoria: Clinical presentations and challenges experienced by a multidisciplinary team and gender service’. Human Systems, 1(1), 70–95. [Link] ↩︎
- Littman, L. (2018). Rapid-onset gender dysphoria in adolescents and young adults: A study of parental reports. PLOS ONE, 13 (8). [Link] ↩︎
- Mazaheri Meybodi, A., Hajebi, A., & Ghanbari Jolfaei, A. (2014). Psychiatric Axis I: Comorbidities among Patients with Gender Dysphoria. Psychiatry journal 2014. [Link] ↩︎
- de Freitas, L. D., Léda-Rêgo, G., Bezerra-Filho, S., & Miranda-Scippa, Â. (2020). Psychiatric disorders in individuals diagnosed with gender dysphoria: A systematic review. Psychiatry and Clinical Neurosciences, 74 (2), 99–104. [Link] ↩︎
-
People with an incongruent gender identity are over four times more likely than the general population to suffer from mental health problems
This finding, from an American campus survey1, found that gender minority status was associated with “4.3 times higher odds of having at least 1 mental health problem.” Similarly, a Journal of Sex and Marital Therapy article2 notes that “a large percentage of adolescents referred for gender dysphoria have a substantial co-occurring history of psychosocial and psychological vulnerability.”
In Lisa Littman’s seminal work3 on rapid onset gender dysphoria, 62.5% of the young people whose parents were surveyed had at least one mental health or neurodevelopmental issue. 58.0% had a poor or extremely poor ability to handle negative emotions productively; 61.4% were overwhelmed by strong emotions and tried to avoid (or went to great lengths to avoid) experiencing them.
In a systematic review4 of individuals diagnosed with gender dysphoria, 53.2% had at least one mental disorder in their lifetime. Such figures substantially exceed prevalence rates of comorbid psychopathology in the general population5: a further paper6 studying hospital encounters found that the prevalence of mental disorder diagnoses was higher in transgender encounters (77%) than in the general population (37.8%).
A Swedish study7 found that sex-reassigned persons had a higher risk of inpatient care for a psychiatric disorder (other than gender identity disorder) than the control population. Inpatient care for psychiatric disorders was also significantly more common among sex-reassigned persons than among controls, both before and after sex reassignment.
- Lipson, S. K., Raifman, J., Abelson, S. & Reisner, S. L. (2019). Gender Minority Mental Health in the U.S.: Results of a National Survey on College Campuses. American Journal of Preventive Medicine 57 (3): 293-301. [Link] ↩︎
- Bechard, M., VanderLaan, D. P., Wood, H., Wasserman, L. & Zucker, K. (2017). Psychosocial and Psychological Vulnerability in Adolescents with Gender Dysphoria: A “Proof of Principle” Study. Journal of Sex & Marital Therapy 43 (7). [Link] ↩︎
- Littman, L. (2018). Rapid-onset gender dysphoria in adolescents and young adults: A study of parental reports. PLOS ONE, 13 (8). [Link] ↩︎
- de Freitas, L. D., Léda-Rêgo, G., Bezerra-Filho, S., & Miranda-Scippa, Â. (2020). Psychiatric disorders in individuals diagnosed with gender dysphoria: A systematic review. Psychiatry and Clinical Neurosciences, 74 (2), 99–104. [Link] ↩︎
- Zucker, K.J., Lawrence, A.A., Kreukels, B.P. (2016). Gender Dysphoria in Adults. Annu Rev Clin Psychol. 12: 217-47. [Link] ↩︎
- Bishoy, H., Repack, D., Tarang, P., Guirguis, E., Kumar, G. & Sachdeva, R. (2019). Psychiatric disorders in the U.S. transgender population. Annals of Epidemiology 39: 1-7. [Link] ↩︎
- Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L. V., Långström, N., & Landén, M. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study in Sweden. PLoS ONE, 6(2). [Link] ↩︎
-
Children with ADHD are far more likely than average to express gender variance
A study on children1 found that, as compared to non-referred comparisons, participants with ADHD were 6.64 times more likely to express gender variance than participants without ADHD. The study also found that, in cases of ADHD, this gender variance was related to elevated emotional symptoms.
- Strang, J.F., Kenworthy, L., Dominska, A., Sokoloff, J., Kenealy, L.E., Berl, M., Walsh, K., Menvielle, E., Slesaransky-Poe, G., Kim, K.E., Luong-Tran, C., Meagher, H. & Wallace, G.L. (2014) Increased gender variance in autism spectrum disorders and attention deficit hyperactivity disorder. Arch Sex Behav 43 (8): 1525-33. [Link] ↩︎
-
Roughly 15% of transmasculine and transfeminine youths in one study had attention deficit disorders
A study1 which used electronic medical records to identify transmasculine and transfeminine youths found attention deficit disorders in 15% of males and 16% of females.
- Becerra-Culqui, T.A. Liu, Y., Nash, R., Cromwell, L., Flanders, W.D., Getahun, D. Giammattei, S.V., Hunkeler, E.M., Lash, T.L., Millman, A., Quinn, V.P., Robinson, B., Roblin, D., Sandberg, D.E., Silverberg, M.J., Tangpricha, V. & Goodman, M. (2018). ‘Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics 141(5). [Link] ↩︎
-
Obsessive-compulsive traits are more common in people with gender dysphoria
At least two studies1 2 have found a particular connection between intense interests or repetitive behaviors – associated with autism spectrum disorders – and gender dysphoria.
It has also been noted3 that:
With the intensified public awareness and media coverage of issues concerning gender identity and gender incongruence, distinguishing true gender dysphoria or incongruence from the sexual obsessions of obsessive-compulsive disorder (OCD) is especially important. Although intrusive sexual obsessions are not uncommon in OCD, obsessions concerning sexual content are more difficult for clinicians to identify as OCD than other types of obsessions (e.g., obsessions concerning contamination).
- Zucker, K.J., Nabbijohn, A.N., Santarossa, A., Wood, H., Bradley, S.J., Matthews, J., & VanderLaan, D.P. (2017). Intense/obsessional interests in children with gender dysphoria: a cross-validation study using the Teacher’s Report Form. Child and adolescent psychiatry and mental health 11, 51. [Link] ↩︎
- VanderLaan, D.P., Postema, L., Wood, H., Singh, D., Fantus, S., Hyun, J., Leef, J., Bradley, S.J. & Zucker, K.J.. (2015). Do children with gender dysphoria have intense/obsessional interests? J Sex Res. 52 (2): 213-9. [Link] ↩︎
- Safer, D., Bullock, K. & Safer, J. (2016). Obsessive-Compulsive Disorder Presenting as Gender Dysphoria/Gender Incongruence: A Case Report and Literature Review. AACE Clinical Case Reports 2. [Link] ↩︎
-
Children referred to the UK’s largest gender clinic were vastly more likely than average to present with autistic traits
One study1 noted that:
48% of children and young people who were seen in GIDS and whose parents completed the social responsiveness scale (SRS), a quantitative measure of autistic behaviours in children and young people, scored in the mild to severe range.
A BMJ paper2 reported:
Around 35% of referred young people [i.e. referred to the GIDS] present with moderate to severe autistic traits.
- Churcher Clarke, A. & Spiliadis, A. (2019). ‘Taking the lid off the box’: The value of extended clinical assessment for adolescents presenting with gender identity difficulties. Clin Child Psychol Psychiatry 24 (2): 338-352. [Link] ↩︎
- Butler, G., De Graaf, N., Wren, B. & Carmichael, P. (2018) Assessment and support of children and adolescents with gender dysphoria. Archives of Disease in Childhood103:631-636. [Link] ↩︎
-
One study found that adulthood homosexuality was 8 to 15 times higher for participants with a history of gender variance
In a 20-year follow-up1 of children, it was found that adulthood homosexuality was 8 to 15 times higher for participants with a history of gender variance.
-
According to a long-range study, around 6% of children in the population are gender variant
Epidemiological study1 based on data from 1983-2007 shows that 6% of children in the population are gender variant.
- Steensma, T.D., van der Ende, J., Verhulst, F.C. & Cohen‐Kettenis, P.T. (2013). Gender Variance in Childhood and Sexual Orientation in Adulthood: A Prospective Study. J Sex Med 10 (11): 2723-2733. [Link] ↩︎
-
Between 2007 and 2017, the number of transgender youth clinics in the US went from 1 to at least 41 – and the number continues to increase
A 2017 paper1 notes that:
The first transgender youth clinic in the United States opened in Boston in 2007. Since then, 40 other clinics have opened that cater exclusively to children, with new clinic openings being announced frequently.
- Marchiano, L. (2017). Outbreak: On Transgender Teens and Psychic Epidemics. Psychological Perspectives 60 (3): 345-366. [Link] ↩︎
-
The profile of people seeking transition has shifted drastically, from overwhelmingly middle-aged males to predominantly adolescent females
A 2017 paper1 notes that “in adolescents, there has been a recent inversion in the sex ratio from one favouring birth-assigned males to one favouring birth-assigned females.” By contrast, over 90% of transsexual adults in the 1960s were male2.
In fact, there was hardly any scientific literature before 2012 on girls ages 11 to 21 ever having developed gender dysphoria at all. Yet of the young people described in Lisa Littman’s 2018 seminal paper on young people3, 82.8% were female.
The data for the UK’s Gender Identity Development Service4 show that 138 children were referred in 2011, and most of those children were boys. By 2021, however, a complete sex ratio reversal had occurred, and the clinic saw 2383 children that year, with almost 70% being female.
A 2017 article by Lisa Marchiano5 collated data from different clinics around the world and found international evidence for this shift in distribution.
- Zucker, K. J. (2017). Epidemiology of gender dysphoria and transgender identity. Sexual Health 14 (5): 404-411. [Link] ↩︎
- Barrett, J. (2015). Written evidence submitted by British Association of Gender Identity Specialists to the Transgender Equality Inquiry. data.parliament.uk [Link] ↩︎
- Littman, L. (2018). Rapid-onset gender dysphoria in adolescents and young adults: A study of parental reports. PLOS ONE, 13 (8). [Link] ↩︎
- Gender Identity Development Service (2021). Referrals to GIDS, financial years 2010-11 to 2020-21. [Link] ↩︎
- Marchiano, L. (2017). Outbreak: On Transgender Teens and Psychic Epidemics. Psychological Perspectives 60 (3): 345-366. [Link] ↩︎
-
The District of Columbia has three and a half times more people who identify as trans than any State in the US, per head of the population
A Williams Institute survey1 found that 2.77% of the population of DC identified as trans – more than three and a half times as many as Hawaii, which (at 0.78%) had the highest proportion of trans people of all fifty States.
- Flores, A.R., Herman, J. L.; Gates, G. J. & Brown, T.N.T. (2016). How many people are lesbian, gay, bisexual, and transgender? Los Angeles, CA: The Williams Institute. [Link] ↩︎
-
In 2018, one study noted that the estimated number of young people who identified as transgender ranged between 0.17% and 1.3%
A 2018 paper1 presented the results of North American studies using short (one to three item) self-reports of gender identity and its variance. The studies suggested that 0.17%–1.3% of adolescents and young adults identified as transgender.
Statistics for the transgender population are almost impossible to quantify as different definitions are used to describe the term ”transgender”. We have chosen this study for its reliability and its reasonable understanding of the term “transgender” in the twenty-first century.
- Kaltiala-Heino, R., Bergman, H., Työläjärvi, M., & Frisén, L. (2018). Gender dysphoria in adolescence: current perspectives. Adolescent health, medicine and therapeutics 9, 31–41. [Link] ↩︎
-
There has been a roughly twenty-fold rise in the number of people seeking transition, with teenagers hugely over-represented
A 2017 paper1 reports that “the prevalence of a self-reported transgender identity in children, adolescents and adults ranges from 0.5 to 1.3%, markedly higher than prevalence rates based on clinic-referred samples of adults.”
This is reflected in data from gender clinics. The UK’s Gender Identity Development Service reported2 a twenty-fold increase in referrals over the course of the last decade:

This surge was primarily driven by adolescents, with 15 being the most common age of referral:

Similarly, a Dutch gender identity clinic reported3 a twenty-fold increase, albeit over a longer time span: from 34 in 1980 to 686 in 2015:

New Zealand4, Finland5 and Canada6 have recorded similar dramatic exponential increases.
- Zucker, K. J. (2017). Epidemiology of gender dysphoria and transgender identity. Sexual Health 14 (5): 404-411. [Link] ↩︎
- Gender Identity Development Service (2021). Referrals to GIDS, financial years 2010-11 to 2020-21. [Link] ↩︎
- Wiepjes, C.M., Nota, N.M., de Blok, C.J.M., Klaver, M., de Vries, A.L.C., Wensing-Kruger, S.A., de Jongh, R.T., Bouman, M.B., Steensma, T.D., Cohen-Kettenis, P., Gooren, L.J.G., Kreukels, B.P.C. & den Heijer, M. (2018). The Amsterdam Cohort of Gender Dysphoria Study (1972-2015): Trends in Prevalence, Treatment, and Regrets. Journal of Sexual Medicine 15 (4). [Link] ↩︎
- Delahunt, J.W., Denison, H.J., Sim, D.A., Bullock, J.J. & Krebs, J.D. (2018). Increasing rates of people identifying as transgender presenting to Endocrine Services in the Wellington region. N Z Med J 131: 33-42. [Link] ↩︎
- Kaltiala-Heino, R., Sumia, M., Työläjärvi, M. & Lindberg, N. (2015). Two years of gender identity service for minors: overrepresentation of natal girls with severe problems in adolescent development. Child and Adolescent Psychiatry and Mental Health 9 (1). [Link] ↩︎
- Aitken, M., Steensma, T.D., Blanchard, R., VanderLaan, D.P., Wood, H., Fuentes, A., Spegg, C., Wasserman, L., Ames, M., Fitzsimmons, C.L., Leef, J.H., Lishak, V., Reim, E., Takagi, A., Vinik, J., Wreford, J., Cohen-Kettenis, P.T., de Vries, A.L., Kreukels, B.P. & Zucker, K.J. (2015). Evidence for an altered sex ratio in clinic-referred adolescents with gender dysphoria. J Sex Med 12 (3): 756-63. [Link] ↩︎
-
From 2010 to 2020, four patients were known or suspected to have died by suicide, out of about 15,000 patients (including those on the waiting list)
Two of these patients were on the waiting list, while two were receiving treatment at the Gender Identity Development Service (GIDs) at the Tavistock.
This gives a suicide rate of 0.03%.1 This is in keeping with the suicide rate for youths with other mental health difficulties.
- Biggs, M. (2022) Suicide by Clinic-Referred Transgender Adolescents in the United Kingdom. Arch Sex Behav 51, 685–690. [Link] ↩︎



